Pregnancy Basics
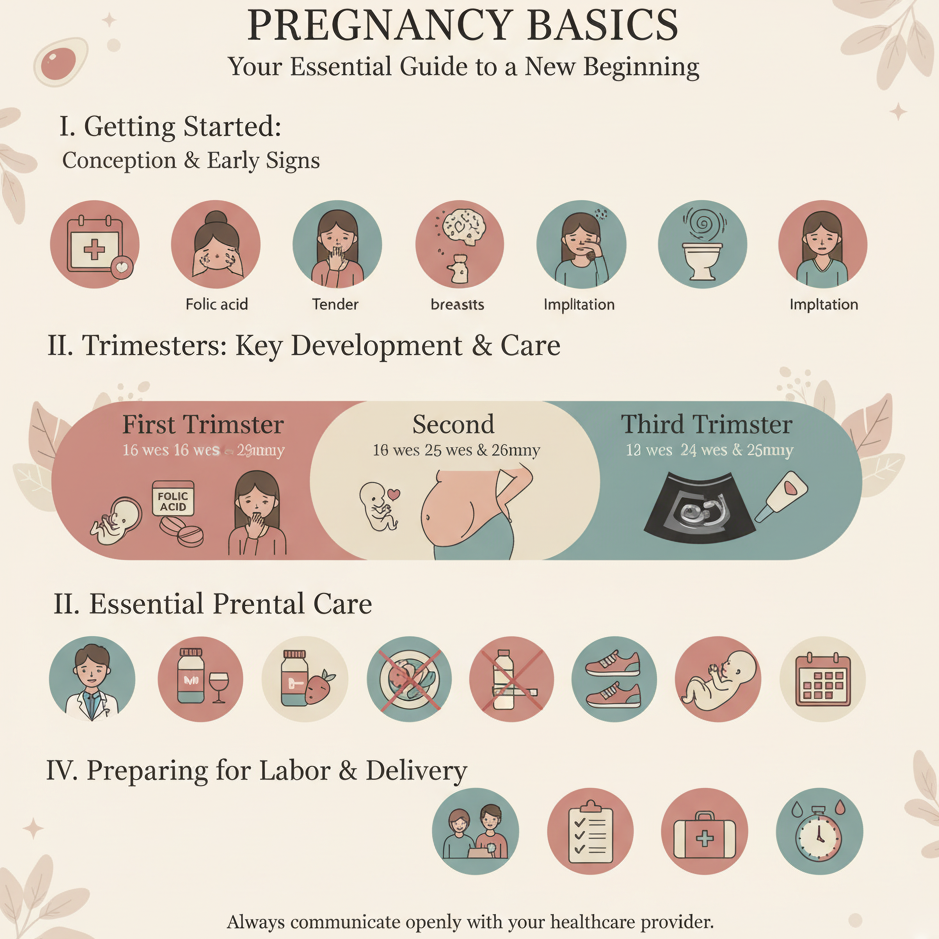
Understanding the basics of pregnancy equips expectant parents with the knowledge to navigate this transformative journey. This guide covers the stages of pregnancy, essential health practices, and tracking tips to support maternal and fetal well-being. Always consult a healthcare provider to personalize your pregnancy care, especially if you have specific health conditions or concerns.
1. Overview of Pregnancy Stages
Pregnancy lasts approximately 40 weeks, divided into three trimesters, each with distinct developmental milestones for the baby and physical/emotional changes for the mother.
-
First Trimester (Weeks 1–12):
-
Fetal Development: The embryo forms major organs (heart, brain, lungs), with the heart beating by week 6. By week 12, the fetus is about the size of a plum (~5–6 cm).
-
Maternal Changes: Nausea (morning sickness), fatigue, breast tenderness, and frequent urination are common due to hormonal shifts.
-
Key Actions: Schedule a prenatal visit, start folic acid (400–800 mcg daily), and track symptoms like nausea in a notebook or digital reminder system.
-
-
Second Trimester (Weeks 13–26):
-
Fetal Development: The fetus grows rapidly, developing hair, nails, and muscles. Movements (quickening) are felt around weeks 18–20. By week 26, the fetus is about the size of a zucchini (~35 cm).
-
Maternal Changes: Energy often improves, but back pain, round ligament pain, or nasal congestion may occur.
-
Key Actions: Monitor fetal movements (aim for 10 in 2 hours by week 28) and maintain a balanced diet rich in iron and calcium.
-
-
Third Trimester (Weeks 27–40):
-
Fetal Development: The fetus gains weight, lungs mature, and bones harden. By week 40, the baby is about the size of a small pumpkin (~50–52 cm, 6–9 lbs).
-
Maternal Changes: Swelling, shortness of breath, and Braxton Hicks contractions are common as the body prepares for labor.
-
Key Actions: Create a birth plan, pack a hospital bag, and track fetal movements daily.
-
-
Purpose: Understanding stages helps you anticipate changes and align care with fetal and maternal needs.
2. Essential Health Practices
-
Nutrition:
-
Eat a balanced diet with vegetables (2.5–3 cups), fruits (1.5–2 cups), whole grains (6–8 oz), protein (70–100 g), and dairy (3 cups) daily.
-
Take a prenatal vitamin with folic acid (400–600 mcg), iron (27 mg), and calcium (1,000 mg).
-
Avoid high-mercury fish (e.g., swordfish), raw/undercooked foods, and alcohol.
-
-
Hydration: Drink 8–10 cups of water daily to support amniotic fluid and reduce swelling.
-
Exercise: Engage in 150 minutes of moderate activity weekly (e.g., walking, prenatal yoga), unless contraindicated by your provider.
-
Sleep: Aim for 7–9 hours nightly, using a pregnancy pillow for comfort, especially in the third trimester.
-
Purpose: Supports fetal development, maternal energy, and reduces complication risks.
3. Prenatal Care Basics
-
Schedule:
-
First visit: Confirm pregnancy and assess health (weeks 6–12).
-
Monthly visits until week 28, biweekly until week 36, then weekly until delivery.
-
-
Key Assessments:
-
Ultrasounds to monitor fetal growth (e.g., around weeks 8–12 and 18–20).
-
Blood tests for anemia, blood type, or infections.
-
Glucose screening (weeks 24–28) for gestational diabetes.
-
-
Tips: Bring a symptom log to visits and ask about vaccinations (e.g., flu, Tdap).
-
Purpose: Ensures early detection of issues and tailored care for mother and baby.
4. Track Symptoms and Milestones
-
Action: Use a notebook, calendar, or digital reminder system to log:
-
Symptoms (e.g., nausea, fatigue, swelling) and their severity.
-
Fetal movements (second trimester onward, aiming for 10 in 2 hours by week 28).
-
Nutrition, exercise, and sleep patterns to monitor wellness.
-
-
Tips:
-
Note patterns (e.g., “Week 20: felt kicks after dinner”) to share with your provider.
-
Track for consistency across trimesters to identify changes or concerns.
-
-
Purpose: Helps monitor health, communicate with your provider, and foster connection with your baby.
5. Manage Common Pregnancy Symptoms
-
Nausea (First Trimester):
-
Eat small, frequent meals (e.g., crackers, bananas) and stay hydrated.
-
-
Back Pain (Second/Third Trimester):
-
Use heat therapy (10–20 minutes, low heat) or gentle stretching.
-
-
Swelling (Third Trimester):
-
Elevate feet, avoid tight clothing, and stay hydrated.
-
-
Fatigue: Take 20–60-minute naps and prioritize sleep hygiene.
-
Purpose: Enhances comfort and supports daily functioning.
6. Emotional and Mental Wellness
-
Techniques:
-
Practice self-love affirmations (e.g., “I am strong and capable”) for 5 minutes daily.
-
Use deep breathing or meditation to reduce stress (5–10 minutes daily).
-
Connect with a support group of expectant parents for shared experiences.
-
-
Tips:
-
Journal emotions or concerns to process changes.
-
Discuss feelings with your partner to build mutual support.
-
-
Purpose: Reduces stress-related risks and promotes emotional resilience.
7. Involve Your Partner or Support System
-
Action:
-
Share tracking responsibilities (e.g., logging fetal movements) with your partner.
-
Discuss birth plans, wellness goals, and emotional needs together.
-
-
Tips:
-
Attend prenatal visits as a team to stay informed.
-
Plan healthy meals or relaxation activities together.
-
-
Purpose: Strengthens partnership and fosters a supportive pregnancy environment.
8. Know When to Seek Medical Advice
-
Warning Signs:
-
Vaginal bleeding, severe abdominal pain, or reduced fetal movement.
-
Sudden swelling, severe headaches, or vision changes (possible preeclampsia).
-
Regular contractions before 37 weeks (possible preterm labor).
-
-
Action: Contact your healthcare provider immediately for concerning symptoms.
-
High-Risk Pregnancies: If you have conditions like hypertension or diabetes, discuss a tailored monitoring plan.
-
Purpose: Ensures timely intervention for maternal or fetal health concerns.
Benefits
-
Healthy Pregnancy: Supports optimal fetal growth and maternal well-being.
-
Informed Decisions: Equips you with knowledge to navigate pregnancy confidently.
-
Emotional Connection: Enhances bonding through tracking and awareness of milestones.
Practical Tips
-
Tracking Tools: Log symptoms, movements, and wellness practices in a journal (e.g., “Week 15: mild nausea, ate spinach salad”). Include details for provider visits.
-
Nutrition Prep: Keep nutrient-rich snacks (e.g., nuts, fruit) handy for energy and nausea management.
-
Exercise Safety: Choose pregnancy-safe activities (e.g., swimming) and stay hydrated during workouts.
-
Rest Environment: Use a pregnancy pillow and keep your bedroom cool (60–68°F) for better sleep.
-
Emergency Plan: Save your provider’s contact info and a nearby hospital’s number for quick access.
-
Support System: Schedule weekly check-ins with your partner or loved ones to discuss progress and needs.
Actionable Next Steps
-
Today: Choose a tracking tool and log your due date, symptoms, or wellness practices. Start a prenatal vitamin with folic acid.
-
This Week: Schedule your first prenatal visit and plan a balanced meal with key nutrients.
-
Ongoing: Track symptoms and fetal movements across trimesters. Consult your provider for any concerns or to tailor your care plan.
Related Articles

Week 19 - Muscle Development

Week 7 - Facial Features Form

Week 8 - Major Organs Develop

Ovulation Prediction

Week 32 - Nail Growth

Week 30 - Head Hair Thickens
Week 1 - Early Pregnancy

Week 37 - Full-Term Begins