Mood Swing Support

Mood swings during the menstrual cycle or pregnancy are often driven by hormonal fluctuations, stress, or physical discomfort. This guide provides practical strategies to stabilize emotions, reduce irritability, and promote emotional resilience during these periods. Always consult a healthcare provider if mood swings are severe, persistent, or accompanied by signs of anxiety or depression, especially during pregnancy.
1. Understand Mood Swings in Cycle and Pregnancy
-
Menstrual Cycle:
-
Menstrual Phase (Days 1–5): Low estrogen and progesterone may cause irritability or fatigue.
-
Follicular Phase (Days 1–13): Rising estrogen often improves mood, but stress can still trigger fluctuations.
-
Ovulation Phase (Day 14, varies): Estrogen peaks may boost energy but can also cause emotional sensitivity in some.
-
Luteal Phase (Days 15–28): Progesterone rise and premenstrual syndrome (PMS) can lead to irritability, sadness, or anxiety.
-
-
Pregnancy:
-
First Trimester (Weeks 1–12): Rapid hormonal changes (e.g., rising hCG, estrogen) may cause mood swings, anxiety, or tearfulness.
-
Second Trimester (Weeks 13–26): Stabilizing hormones often improve mood, but body changes or stress can cause fluctuations.
-
Third Trimester (Weeks 27–40): Fatigue, discomfort, or anticipation of labor may increase emotional sensitivity.
-
-
Purpose: Recognizing when and why mood swings occur helps tailor support strategies to specific phases.
2. Practice Emotional Regulation Techniques
-
Deep Breathing:
-
Inhale for 4 seconds, hold for 4 seconds, exhale for 6 seconds. Repeat for 5 minutes during emotional peaks.
-
Use during PMS or pregnancy anxiety to calm the nervous system.
-
-
Mindfulness Meditation:
-
Focus on your breath or a calming word (e.g., “peace”) for 5–10 minutes daily.
-
Helps manage luteal phase irritability or pregnancy-related stress.
-
-
Self-Love Affirmations:
-
Repeat positive statements (e.g., “I am calm and capable”) for 2–5 minutes daily, especially during PMS or early pregnancy.
-
-
Purpose: Reduces emotional intensity and promotes a sense of control.
3. Maintain a Balanced Lifestyle
-
Nutrition:
-
Eat complex carbs (e.g., oats, quinoa) and protein (e.g., eggs, beans) to stabilize blood sugar, which impacts mood.
-
Include magnesium-rich foods (e.g., almonds, spinach) to reduce PMS-related irritability.
-
Limit caffeine (under 200 mg daily) and avoid alcohol to prevent mood disruptions.
-
-
Exercise:
-
Engage in 150 minutes of moderate activity weekly (e.g., walking, prenatal yoga for pregnancy) to release endorphins.
-
Avoid intense exercise during heavy menstrual flow or late pregnancy unless approved by your provider.
-
-
Sleep:
-
Aim for 7–9 hours nightly, with a consistent bedtime routine to support hormonal balance.
-
Use a warm bath or heat therapy before bed during menstruation to ease cramps and promote relaxation.
-
-
Purpose: Supports physical health, which directly influences emotional stability.
4. Track Mood and Triggers
-
Action: Use a notebook, calendar, or digital reminder system to log:
-
Mood swings (e.g., “Day 20: felt irritable, luteal phase”).
-
Triggers (e.g., lack of sleep, stress, diet).
-
Coping strategies and their effectiveness (e.g., “5-min meditation, felt calmer”).
-
Cycle or pregnancy symptoms (e.g., cramps, fatigue) to identify patterns.
-
-
Tips:
-
Track daily for 3–6 cycles or throughout pregnancy to spot trends (e.g., worse moods in luteal phase).
-
Note improvements or persistent issues for provider discussions.
-
-
Purpose: Helps identify mood swing patterns and effective strategies, aiding communication with healthcare providers.
5. Use Relaxation Techniques
-
Progressive Muscle Relaxation (PMR):
-
Tense and relax each muscle group (e.g., shoulders, arms) for 5–10 seconds over 10 minutes to reduce tension.
-
Ideal for luteal phase anxiety or pregnancy discomfort.
-
-
Journaling:
-
Write about emotions or stressors for 5–10 minutes daily to process feelings.
-
Use prompts like “What made me feel supported today?” to focus on positives.
-
-
Warm Baths:
-
Soak in a warm bath (95–100°F or 35–38°C) for 15 minutes to relax during menstruation or pregnancy (avoid hot baths in pregnancy).
-
-
Purpose: Reduces stress and emotional volatility, enhancing mood stability.
6. Connect with a Support System
-
Action:
-
Share mood swing experiences with your partner, family, or friends to gain emotional support.
-
Join local or online groups for menstruating individuals or expectant parents to share coping strategies.
-
-
Tips:
-
Discuss specific triggers (e.g., PMS, pregnancy fatigue) to foster understanding.
-
Schedule regular check-ins to maintain open communication.
-
-
Purpose: Reduces feelings of isolation and provides emotional reinforcement.
7. Know When to Seek Medical Advice
-
Warning Signs:
-
Severe or persistent mood swings that disrupt daily life, relationships, or work.
-
Signs of anxiety (e.g., constant worry) or depression (e.g., persistent sadness, loss of interest).
-
Mood changes accompanied by physical symptoms like irregular cycles, severe cramps, or reduced fetal movement (in pregnancy).
-
-
Action: Consult a healthcare provider if mood swings persist beyond a cycle or trimester or feel overwhelming.
-
High-Risk Pregnancies: If you have conditions like gestational diabetes or a history of mental health issues, discuss mood management plans with your provider.
-
Purpose: Ensures timely evaluation for conditions like premenstrual dysphoric disorder (PMDD), perinatal depression, or hormonal imbalances.
Benefits
-
Emotional Stability: Reduces the intensity and frequency of mood swings.
-
Hormonal Balance: Supports cycle regularity and pregnancy health by lowering stress.
-
Improved Well-Being: Enhances confidence and resilience during hormonal changes.
Practical Tips
-
Tracking Tools: Log mood swings and coping strategies in a journal (e.g., “Day 25: felt anxious, 5-min breathing helped”). Include cycle or pregnancy phase for context.
-
Routine Integration: Schedule 5–10 minutes daily for relaxation (e.g., meditation, affirmations) during high-risk phases (luteal, first trimester).
-
Nutrition Support: Keep nutrient-rich snacks (e.g., bananas, yogurt) handy to stabilize blood sugar during mood dips.
-
Environment Setup: Create a calming space with soft lighting or music for relaxation techniques.
-
Partner Involvement: Share mood logs or practice affirmations together to build mutual support.
-
Emergency Plan: Keep your provider’s contact info accessible for urgent mood-related concerns.
Actionable Next Steps
-
Today: Choose a tracking tool and log your current mood and cycle/pregnancy phase. Try a 5-minute deep breathing exercise.
-
This Week: Test 2–3 techniques (e.g., affirmations, journaling) and note their impact on mood.
-
Next 3–6 Cycles or Trimesters: Track mood swings and coping strategies consistently. Adjust techniques based on effectiveness.
-
Ongoing: Consult a healthcare provider if mood swings are severe, persistent, or disrupt daily life.
Related Articles

Exercise for Period Pain

Week 22 - Lung Maturation

Week 14 - Bones Harden

Week 37 - Full-Term Begins

Period calculator
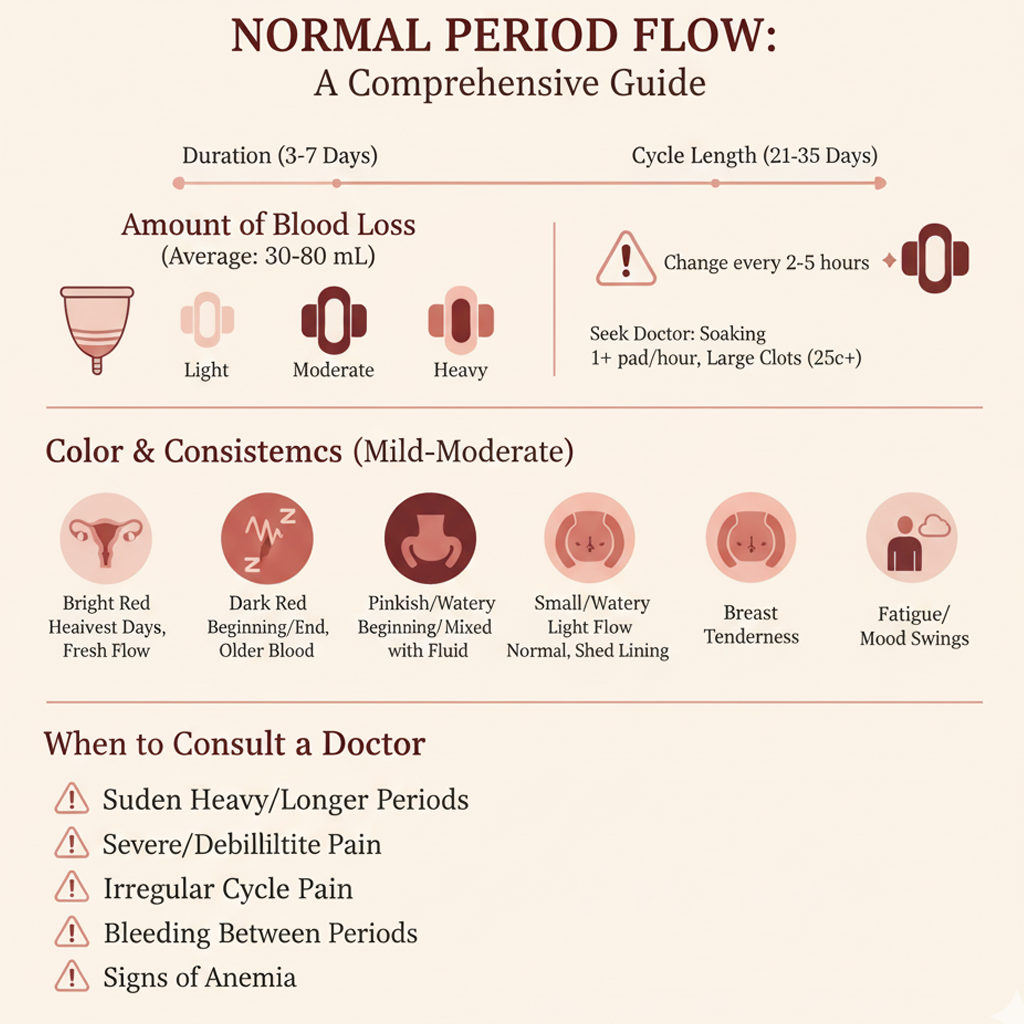
Normal Period Flow

Pregnancy Test Calculator
Fertility Test Basics: Your Guide to Tracking Pregnancy