Pregnancy Food Guide
A balanced, nutrient-rich diet during pregnancy supports maternal health, fetal development, and overall well-being. This guide outlines key food groups, portion recommendations, and safety tips to optimize nutrition across all trimesters. Always consult a healthcare provider to tailor your diet, especially if you have conditions like gestational diabetes, food allergies, or dietary restrictions.
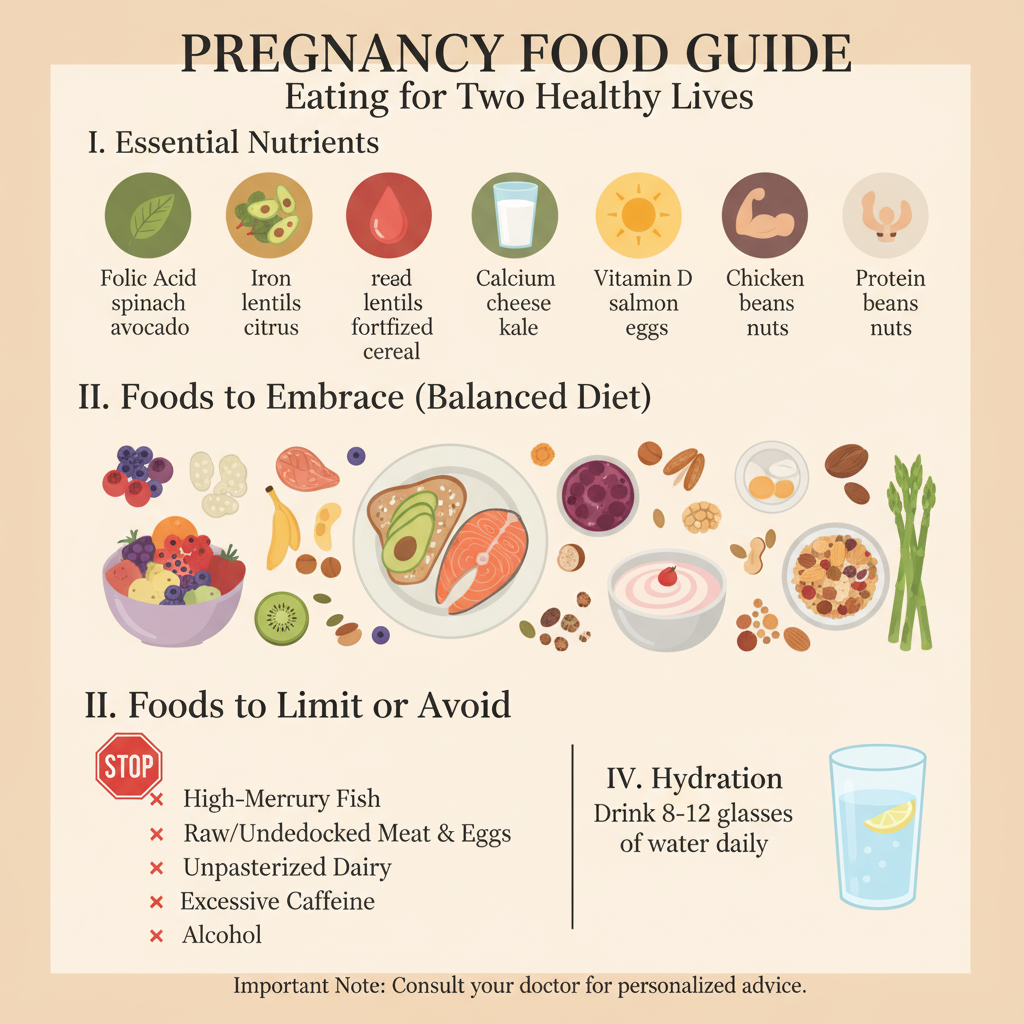
1. Key Nutrients and Food Sources
Focus on these essential nutrients to support pregnancy health:
-
Folic Acid (400–800 mcg daily):
-
Role: Prevents neural tube defects and supports early fetal brain development.
-
Sources: Leafy greens (spinach, kale), legumes (lentils, black beans), citrus fruits (oranges), and fortified grains (bread, pasta).
-
Supplement: Take a prenatal vitamin with 400–600 mcg folic acid daily, starting preconception if possible.
-
-
Iron (27 mg daily):
-
Role: Supports increased blood volume and prevents anemia.
-
Sources: Lean meats (chicken, beef), fish, spinach, lentils, and fortified cereals. Pair with vitamin C-rich foods (e.g., bell peppers, strawberries) to enhance absorption.
-
-
Calcium (1,000 mg daily):
-
Role: Builds fetal bones and teeth, supports maternal bone health.
-
Sources: Dairy (milk, yogurt, cheese), fortified plant-based milk (soy, almond), broccoli, and almonds.
-
-
Protein (70–100 g daily):
-
Role: Supports fetal tissue growth and maternal energy needs.
-
Sources: Lean meats, poultry, fish, eggs, tofu, beans, and nuts.
-
-
Omega-3 Fatty Acids (200–300 mg DHA daily):
-
Role: Promotes fetal brain and eye development.
-
Sources: Fatty fish (salmon, mackerel), walnuts, chia seeds, and flaxseeds.
-
-
Purpose: Ensures adequate nutrition for fetal growth and maternal health across trimesters.
2. Recommended Food Groups and Portions
Incorporate a variety of foods daily to meet nutritional needs:
-
Vegetables (2.5–3 cups):
-
Include a mix of colors: leafy greens (spinach), orange vegetables (carrots, sweet potatoes), and cruciferous vegetables (broccoli).
-
Aim for raw or lightly cooked to retain nutrients.
-
-
Fruits (1.5–2 cups):
-
Choose fresh or frozen fruits like berries, apples, or bananas. Limit fruit juice to avoid excess sugar.
-
-
Whole Grains (6–8 oz):
-
Opt for whole-grain bread, brown rice, quinoa, or oats for fiber and sustained energy.
-
-
Protein Foods (5–6.5 oz):
-
Include lean meats, poultry, fish, eggs, beans, or tofu. Aim for 2–3 servings of fish weekly (low-mercury options like salmon).
-
-
Dairy or Alternatives (3 cups):
-
Choose milk, yogurt, or fortified plant-based alternatives for calcium and vitamin D.
-
-
Healthy Fats:
-
Use olive oil, avocado, or nuts in moderation for heart health and fetal development.
-
-
Purpose: Provides balanced nutrition to support energy, growth, and pregnancy demands.
3. Food Safety Guidelines
-
Avoid High-Risk Foods:
-
Raw or undercooked meat, poultry, fish (e.g., sushi), or eggs to prevent foodborne illnesses like listeria or salmonella.
-
Unpasteurized dairy or juices, which may contain harmful bacteria.
-
High-mercury fish (e.g., swordfish, shark, king mackerel). Limit tuna to 6 oz weekly.
-
-
Safe Preparation:
-
Wash all produce thoroughly under running water.
-
Cook meats to safe internal temperatures (e.g., poultry to 165°F/74°C, beef to 160°F/71°C).
-
Store perishables below 40°F (4°C) to prevent bacterial growth.
-
-
Caffeine: Limit to under 200 mg daily (about one 8 oz cup of coffee) to minimize risks to fetal development.
-
Alcohol: Avoid completely to prevent fetal alcohol syndrome and developmental issues.
-
Purpose: Reduces risks of foodborne illness and ensures fetal safety.
4. Track Your Diet
-
Action: Use a notebook, calendar, or digital reminder system to log daily food intake, portion sizes, and any symptoms (e.g., nausea, cravings).
-
Tracking Tips:
-
Record meals and snacks (e.g., “Breakfast: oatmeal with berries, 1 cup milk”).
-
Note nutrient intake (e.g., iron-rich foods, calcium sources) to ensure variety.
-
Track symptoms like nausea or heartburn to identify food triggers and discuss with your provider.
-
-
Purpose: Helps maintain balanced nutrition and identify dietary gaps or issues.
5. Manage Common Pregnancy Symptoms
-
Nausea (First Trimester):
-
Eat small, frequent meals (5–6 daily) to stabilize stomach acid.
-
Choose bland foods like crackers, toast, or bananas.
-
Stay hydrated with water or ginger tea (check for pregnancy-safe blends).
-
-
Heartburn (Second/Third Trimester):
-
Avoid spicy, fatty, or acidic foods (e.g., tomatoes, citrus).
-
Eat smaller portions and avoid lying down immediately after meals.
-
-
Constipation:
-
Increase fiber intake with whole grains, fruits (e.g., prunes), and vegetables.
-
Drink 8–10 cups of water daily to support digestion.
-
-
Purpose: Enhances comfort and supports consistent nutrition despite pregnancy symptoms.
6. Address Special Dietary Needs
-
Vegetarian/Vegan Diets:
-
Ensure adequate protein (tofu, lentils, beans), iron (spinach, fortified cereals), and vitamin B12 (fortified foods or supplements).
-
Consult a healthcare provider for a prenatal vitamin with B12 and iron.
-
-
Gestational Diabetes:
-
Work with your provider or a dietitian to manage blood sugar through balanced carbs (e.g., whole grains) and regular meals.
-
-
Food Allergies: Avoid allergens and seek substitutes (e.g., fortified soy milk for dairy allergies).
-
Purpose: Tailors nutrition to specific needs while maintaining fetal and maternal health.
7. Involve Your Partner or Support System
-
Meal Planning: Collaborate on grocery lists and meal prep to ensure nutrient-rich options are available.
-
Shared Tracking: Discuss dietary goals and symptoms with your partner to align on healthy eating habits.
-
Purpose: Strengthens teamwork and supports consistent nutrition throughout pregnancy.
8. Know When to Seek Medical Advice
-
Warning Signs:
-
Persistent nausea or vomiting preventing food intake.
-
Signs of nutritional deficiencies (e.g., extreme fatigue, dizziness, pale skin).
-
Uncontrolled weight gain or loss (outside provider-recommended ranges).
-
-
Action: Consult a healthcare provider if symptoms interfere with eating, you suspect foodborne illness, or you have concerns about weight or nutrition.
-
Purpose: Ensures timely management of dietary or health issues.
Benefits
-
Fetal Development: Supports healthy growth of the baby’s brain, bones, and organs.
-
Maternal Health: Reduces risks of anemia, fatigue, and pregnancy complications.
-
Energy and Comfort: Enhances well-being and manages symptoms like nausea or constipation.
Practical Tips
-
Meal Planning: Plan weekly meals with a balance of vegetables, proteins, and grains. Prep snacks like cut veggies or nuts for convenience.
-
Tracking Tools: Log daily meals in a journal (e.g., “Lunch: grilled chicken, quinoa, spinach salad”). Note nutrient sources and symptoms for provider discussions.
-
Safe Food Prep: Use separate cutting boards for raw meats and produce to avoid cross-contamination.
-
Hydration: Carry a reusable water bottle to meet daily fluid goals (8–10 cups).
-
Portion Control: Use a small plate to manage portion sizes and avoid overeating, especially in the third trimester.
-
Craving Management: Satisfy cravings with healthy alternatives (e.g., fruit for sweets, nuts for salty snacks) to maintain balance.
Actionable Next Steps
-
Today: Choose a tracking tool to log meals and start taking a prenatal vitamin with 400–600 mcg folic acid.
-
This Week: Plan a balanced menu with iron, calcium, and omega-3-rich foods. Review food safety practices.
-
Ongoing: Track diet and symptoms across trimesters. Consult a healthcare provider for persistent symptoms or dietary concerns.
Related Articles

Week 3 - Germ Layer Formation

Week 21 - Eyebrows Form

Week 29 - Lung Function Improves

Week 30 - Head Hair Thickens
Self-Love Affirmations

Fertility Signs

Week 36 - Descent into Pelvis

Cycle Self-Care Rituals