Cycle Sleep Hygiene
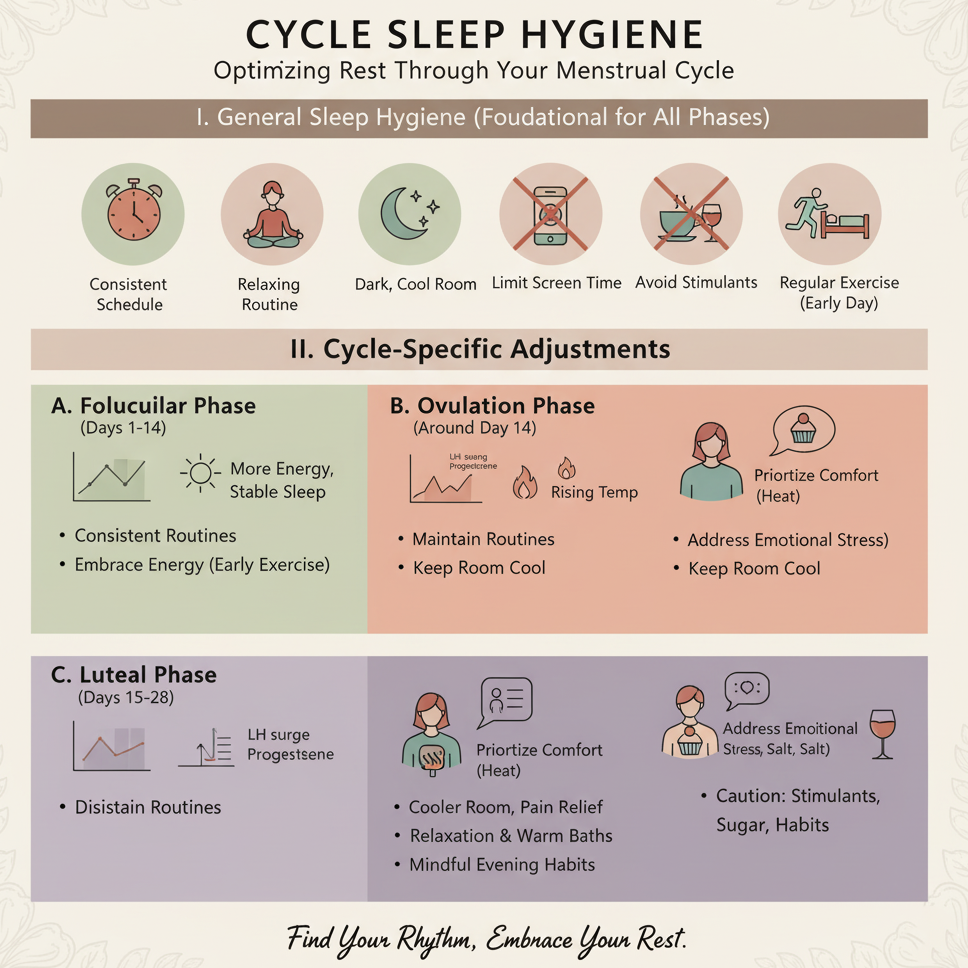
Maintaining good sleep hygiene during the menstrual cycle promotes restful sleep, balances hormones, and supports overall reproductive health. Hormonal fluctuations across cycle phases can disrupt sleep, so tailored strategies can help manage these changes. This guide provides practical steps to optimize sleep during menstruation, follicular, ovulation, and luteal phases. Always consult a healthcare provider if sleep disturbances persist, are severe, or are accompanied by other concerning symptoms.
1. Understand Cycle-Related Sleep Changes
-
Menstrual Phase (Days 1–5):
-
Sleep Impact: Cramps, bloating, or fatigue may disrupt sleep. Lower progesterone levels can reduce sleep quality.
-
Symptoms: Trouble falling asleep, waking due to pain, or feeling unrested.
-
-
Follicular Phase (Days 1–13):
-
Sleep Impact: Rising estrogen levels may improve sleep as energy increases post-menstruation.
-
Symptoms: Generally better sleep, though stress or lifestyle factors can still interfere.
-
-
Ovulation Phase (Day 14, varies):
-
Sleep Impact: Estrogen peaks, but some experience restlessness or vivid dreams due to hormonal shifts.
-
Symptoms: Mild sleep disruptions or increased energy affecting bedtime.
-
-
Luteal Phase (Days 15–28):
-
Sleep Impact: Rising progesterone can promote sleepiness but also cause night sweats or insomnia, especially during premenstrual syndrome (PMS).
-
Symptoms: Difficulty falling/staying asleep, waking early, or feeling unrested.
-
-
Purpose: Recognizing phase-specific sleep changes helps tailor hygiene practices to your cycle.
2. Establish a Consistent Sleep Schedule
-
Action: Aim for 7–9 hours of sleep nightly, going to bed and waking at the same time daily, even during menstruation.
-
Tips:
-
Set a bedtime routine (e.g., start winding down at 10 PM for an 11 PM bedtime).
-
Adjust slightly during the luteal phase or menstruation if fatigue requires earlier rest.
-
-
Purpose: Regulates your body’s internal clock, supporting hormonal balance and cycle regularity.
3. Create a Sleep-Friendly Environment
-
Temperature: Keep your bedroom cool (60–68°F or 16–20°C) to counteract night sweats, especially in the luteal phase.
-
Lighting: Use blackout curtains or a sleep mask to block light, promoting melatonin production.
-
Noise: Minimize disruptions with earplugs or a fan for white noise.
-
Comfort: Use breathable cotton bedding and supportive pillows to ease cramps or bloating discomfort.
-
Purpose: Enhances sleep quality by creating a restful, distraction-free environment.
4. Practice a Pre-Bed Routine
-
Techniques:
-
Spend 10–15 minutes on calming activities, such as deep breathing, gentle stretching, or journaling, to signal relaxation.
-
Avoid screens (phones, tablets) 1–2 hours before bed to reduce blue light exposure, which can suppress melatonin.
-
-
Tips:
-
During menstruation, try heat therapy (10–15 minutes on the lower abdomen) to ease cramps before bed.
-
In the luteal phase, use mindfulness meditation to manage PMS-related anxiety or restlessness.
-
-
Purpose: Prepares your body and mind for restful sleep, minimizing cycle-related disruptions.
5. Support Sleep with Nutrition and Hydration
-
Nutrition:
-
Eat a balanced diet with magnesium-rich foods (e.g., bananas, almonds) and complex carbs (e.g., whole grains) to promote relaxation and stabilize blood sugar.
-
Avoid heavy meals, caffeine (limit to 200 mg daily), or alcohol 4–6 hours before bed, as they can disrupt sleep, especially during the luteal phase.
-
-
Hydration: Drink 8–10 cups of water daily but reduce intake 1–2 hours before bed to minimize nighttime bathroom trips.
-
Tips:
-
Have a light evening snack (e.g., yogurt with fruit) if hungry to avoid blood sugar dips.
-
During menstruation, include iron-rich foods (e.g., spinach) to combat fatigue from blood loss.
-
-
Purpose: Supports restful sleep and reduces cycle-related symptoms like cramps or mood swings.
6. Manage Cycle-Related Sleep Disruptions
-
Menstrual Cramps:
-
Use a warm water bottle or heating pad (10–20 minutes, low heat) before bed to relax uterine muscles.
-
Try gentle yoga poses (e.g., child’s pose) to ease discomfort.
-
-
PMS Insomnia (Luteal Phase):
-
Practice progressive muscle relaxation (PMR) for 10 minutes to reduce tension.
-
Limit stimulating activities (e.g., intense exercise) in the evening.
-
-
Night Sweats:
-
Wear lightweight, breathable clothing and use layered bedding to adjust for temperature changes.
-
-
Purpose: Addresses phase-specific challenges to improve sleep quality and duration.
7. Track Sleep and Cycle Patterns
-
Action: Use a notebook, calendar, or digital reminder system to log:
-
Sleep duration and quality (e.g., “7 hours, woke once due to cramps”).
-
Cycle phase and symptoms (e.g., “Day 3: heavy flow, mild cramps”).
-
Sleep hygiene practices (e.g., pre-bed routine, nutrition) and their effectiveness.
-
-
Tips:
-
Track for 3–6 cycles to identify patterns (e.g., insomnia during luteal phase).
-
Note improvements or persistent issues to discuss with your provider.
-
-
Purpose: Helps optimize sleep strategies and detect underlying issues affecting rest.
8. Involve Your Support System
-
Action:
-
Share your sleep hygiene goals with your partner or family to create a supportive environment (e.g., minimizing noise at night).
-
Discuss cycle-related sleep challenges to foster understanding and teamwork.
-
-
Tips:
-
Ask for help with evening tasks during menstruation to prioritize rest.
-
Join online or community groups for menstruating individuals to share sleep tips.
-
-
Purpose: Enhances accountability and emotional support for better sleep habits.
9. Know When to Seek Medical Advice
-
Warning Signs:
-
Persistent insomnia or poor sleep quality despite good hygiene practices.
-
Severe fatigue, mood swings, or irritability linked to sleep disruptions.
-
Irregular cycles or intense symptoms (e.g., severe cramps, heavy bleeding) affecting sleep.
-
-
Action: Consult a healthcare provider if sleep issues persist for more than a few cycles or significantly impact daily life.
-
Purpose: Ensures evaluation for conditions like insomnia, hormonal imbalances, or underlying disorders (e.g., thyroid issues, PCOS).
Benefits
-
Hormonal Balance: Improves sleep quality, supporting cycle regularity and reproductive health.
-
Reduced Symptoms: Minimizes cycle-related fatigue, mood swings, or cramps.
-
Emotional Well-Being: Enhances mood and resilience during hormonal fluctuations.
Practical Tips
-
Tracking Tools: Log sleep and cycle details in a journal (e.g., “Day 15: 8 hours sleep, felt rested, luteal phase”). Include symptoms and hygiene practices.
-
Bedtime Routine: Start winding down 30 minutes before bed with calming activities (e.g., reading, stretching).
-
Nutrition Timing: Have dinner 2–3 hours before bed and avoid spicy or heavy foods that may disrupt sleep.
-
Comfort Aids: Use a body pillow during menstruation to support cramp-prone areas.
-
Environment Prep: Keep earplugs, a sleep mask, or a fan handy for quick setup in any bedroom.
-
Stress Management: Pair sleep hygiene with 5–10 minutes of meditation or affirmations (e.g., “I rest easily and wake refreshed”) to enhance relaxation.
Actionable Next Steps
-
Today: Choose a tracking tool and log your sleep duration and cycle phase. Set a consistent bedtime.
-
This Week: Create a pre-bed routine with 10 minutes of relaxation (e.g., deep breathing) and adjust your bedroom for comfort.
-
Next 3–6 Cycles: Track sleep patterns and hygiene practices. Test strategies like heat therapy for cramps or PMR for insomnia.
-
Ongoing: Consult a healthcare provider if sleep disruptions persist or worsen.
Related Articles

Pregnancy Goal Setting

Week 19 - Muscle Development

Week 24 - Viability Threshold

Pregnancy Test Calculator
Week 20 - Halfway Point
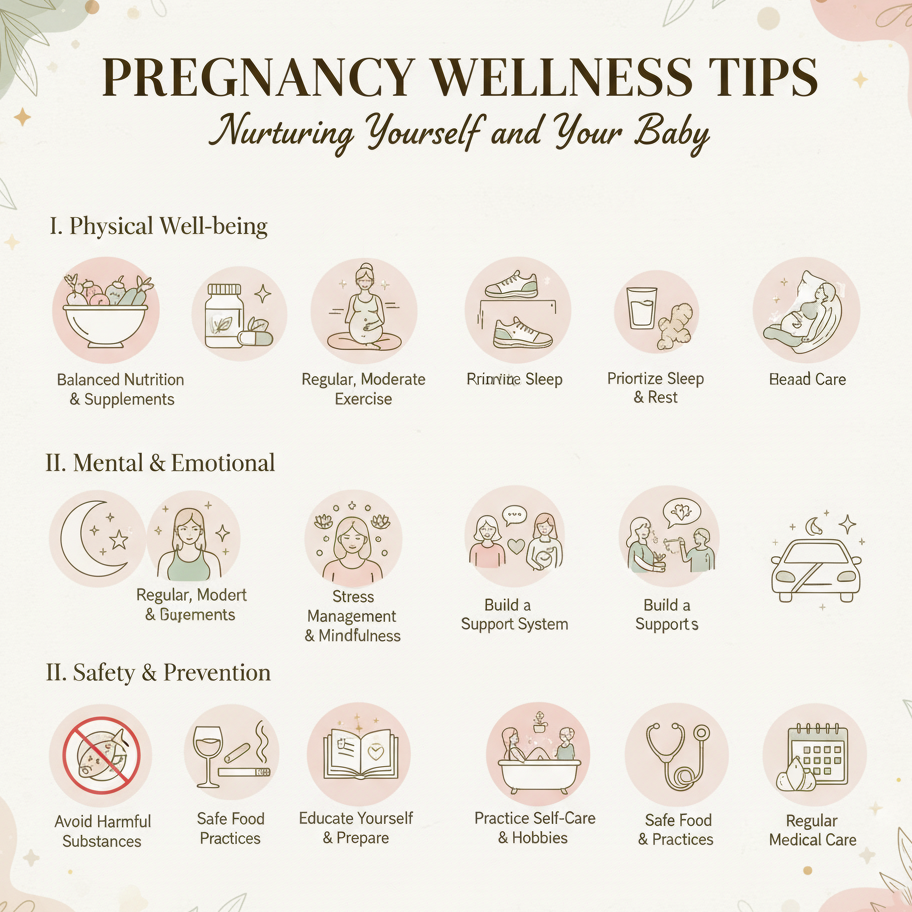
Pregnancy Wellness Tips

Week 38 - Organ Maturation
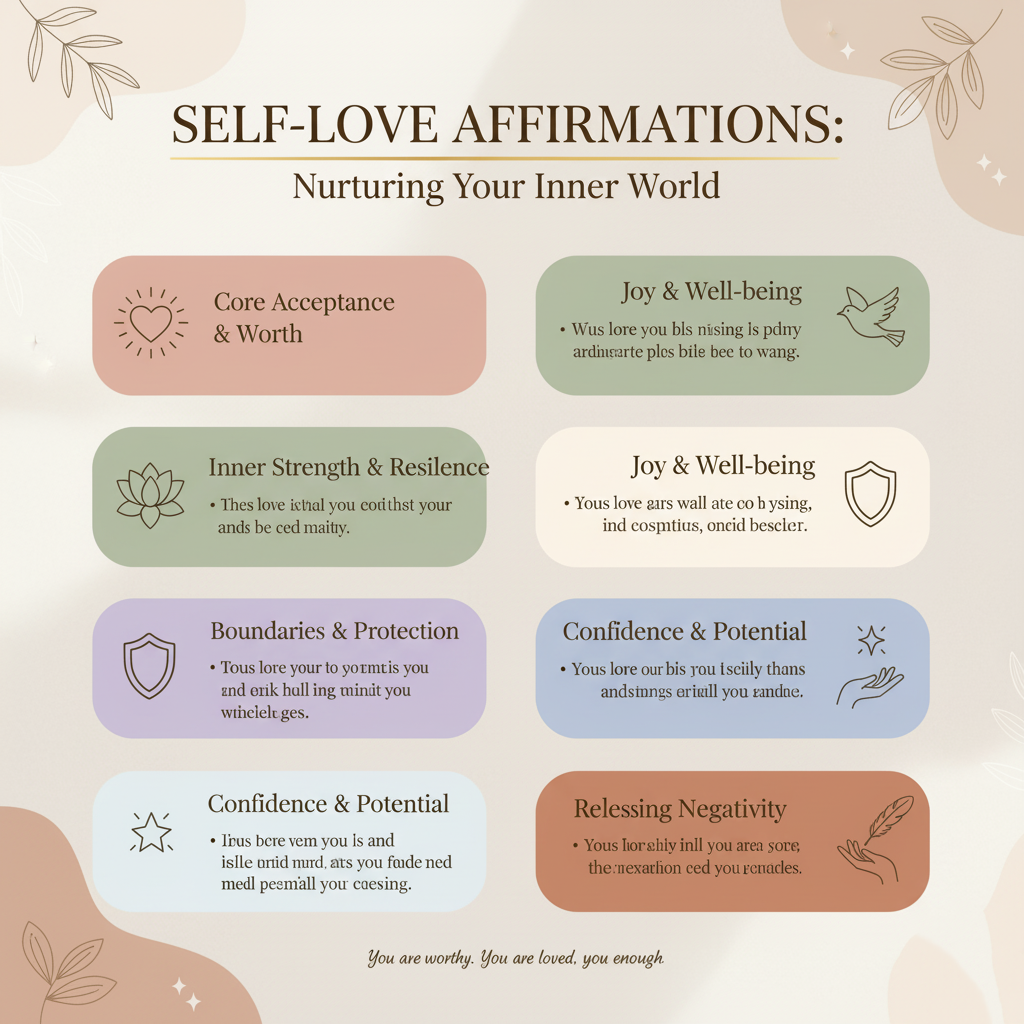
Self-Love Affirmations