Pre-Pregnancy Checklist
A thorough pre-pregnancy checklist establishes a strong foundation for healthy conception and pregnancy. By addressing physical, emotional, and logistical factors, you can optimize fertility and prepare for parenthood. Always consult a healthcare provider to personalize this checklist, especially if you have chronic conditions or specific health concerns.
1. Schedule a Preconception Health Checkup
-
Action: Arrange a visit with a healthcare provider to evaluate your overall health and discuss pregnancy plans.
-
Key Assessments:
-
Review medical history, including chronic conditions (e.g., diabetes, hypertension, or thyroid issues).
-
Update vaccinations (e.g., rubella, varicella) to protect against complications that could affect fetal development.
-
Consider genetic screening to identify carrier status for conditions like cystic fibrosis or sickle cell anemia, especially if there’s a family history.
-
-
Purpose: Identifies and manages health issues that could impact fertility or pregnancy outcomes.
2. Optimize Nutrition and Supplements
-
Folic Acid: Take 400 mcg of folic acid daily, starting at least one month before trying to conceive, to reduce the risk of neural tube defects. Consult your healthcare provider for dosage adjustments if needed.
-
Balanced Diet: Eat a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats (e.g., omega-3s from fish or nuts). Limit processed foods and added sugars.
-
Caffeine: Reduce intake to under 200 mg daily (about one 8 oz cup of coffee) to support fertility.
-
Purpose: Enhances reproductive health and prepares your body for a healthy pregnancy.
3. Achieve a Healthy Weight
-
Goal: Aim for a body mass index (BMI) of 18.5-24.9, as both underweight and overweight conditions can affect fertility.
-
Action: Combine a balanced diet with regular, moderate exercise (e.g., 150 minutes weekly of activities like walking, swimming, or yoga).
-
Purpose: Improves ovulation regularity and reduces pregnancy complications.
4. Eliminate Harmful Substances
-
Quit Smoking: Stop smoking and avoid secondhand smoke, as it can impair fertility and increase miscarriage risk.
-
Eliminate Alcohol: Avoid alcohol to prevent risks to early fetal development.
-
Avoid Recreational Drugs: Discontinue use of any recreational substances, which can harm fertility and pregnancy.
-
Purpose: Minimizes risks to conception and ensures a safer pregnancy.
5. Track Menstrual Cycles
-
Action: Use a notebook, calendar, or digital reminder system to log the start of your periods and track cycle length (typically 21-35 days).
-
Fertile Window: Identify fertile days (e.g., days 10-14 in a 28-day cycle) by monitoring signs like clear, stretchy cervical mucus, a basal body temperature (BBT) rise of 0.5-1°F post-ovulation, or mid-cycle pain.
-
Purpose: Helps time intercourse for conception. Track for 3-6 months to refine accuracy.
6. Incorporate Stress-Reducing Activities
-
Action: Practice daily stress management techniques, such as yoga, meditation, deep breathing, or journaling, to support mental health.
-
Support System: Discuss your plans with your partner or loved ones to build emotional support. Consider joining local or online groups for aspiring parents.
-
Purpose: Reduces stress, which can affect ovulation and fertility.
7. Involve Your Partner
-
Partner’s Health: Encourage your partner to adopt a nutrient-rich diet (e.g., high in zinc, vitamin C, and antioxidants) and healthy lifestyle habits to support sperm health.
-
Shared Planning: Discuss conception goals, timelines, and lifestyle changes together to strengthen your partnership.
-
Health Check: Suggest your partner consult a healthcare provider to assess fertility and overall health.
-
Purpose: Enhances mutual readiness and optimizes conception chances.
8. Monitor for Health Concerns
-
Irregular Cycles: If cycles vary by more than 7 days or fertility signs are absent, consult a healthcare provider to evaluate potential issues like polycystic ovary syndrome (PCOS) or low ovarian reserve.
-
Chronic Conditions: Work with your healthcare provider to manage conditions like diabetes or hypertension before conception.
-
Purpose: Ensures early detection and management of fertility or health issues.
Benefits
-
Lower Miscarriage Risk: Addressing health and lifestyle factors reduces pregnancy complications.
-
Improved Fetal Development: Optimal nutrition and habits support a healthy pregnancy.
-
Confident Transition to Parenthood: Proactive preparation fosters readiness and reduces anxiety.
Practical Tips
-
Tracking Tools: Use a paper calendar or phone-based reminder to log cycle days and fertility signs (e.g., cervical mucus, BBT). Record consistently for reliable patterns.
-
BBT Measurement: Use a digital thermometer (accurate to 0.1°F or 0.1°C) to measure BBT each morning before rising. Track results to confirm ovulation.
-
Nutrition: Include iron-rich foods (e.g., leafy greens, lean meats) and calcium sources (e.g., dairy or fortified alternatives) to support preconception health.
-
Exercise: Engage in moderate activities like walking or prenatal yoga to maintain a healthy weight without overexertion.
-
Stress Management: Try mindfulness exercises or short daily walks to reduce stress. Seek local support groups for aspiring parents if desired.
-
Ovulation Support: Consider over-the-counter ovulation predictor kits to confirm fertile days by detecting the luteinizing hormone (LH) surge. Test during the estimated fertile window and store kits in a cool, dry place.
Actionable Next Steps
-
Today: Schedule a preconception checkup and begin taking 400 mcg of folic acid daily.
-
This Week: Start tracking your menstrual cycle and review your diet, caffeine intake, and lifestyle habits.
-
Next Month: Discuss financial plans and work arrangements with your partner. Confirm vaccination status with your healthcare provider.
-
Ongoing: Track fertility signs for 3-6 months and consult a healthcare provider if you notice irregularities or have trouble conceiving.
Related Articles

Week 14 - Bones Harden
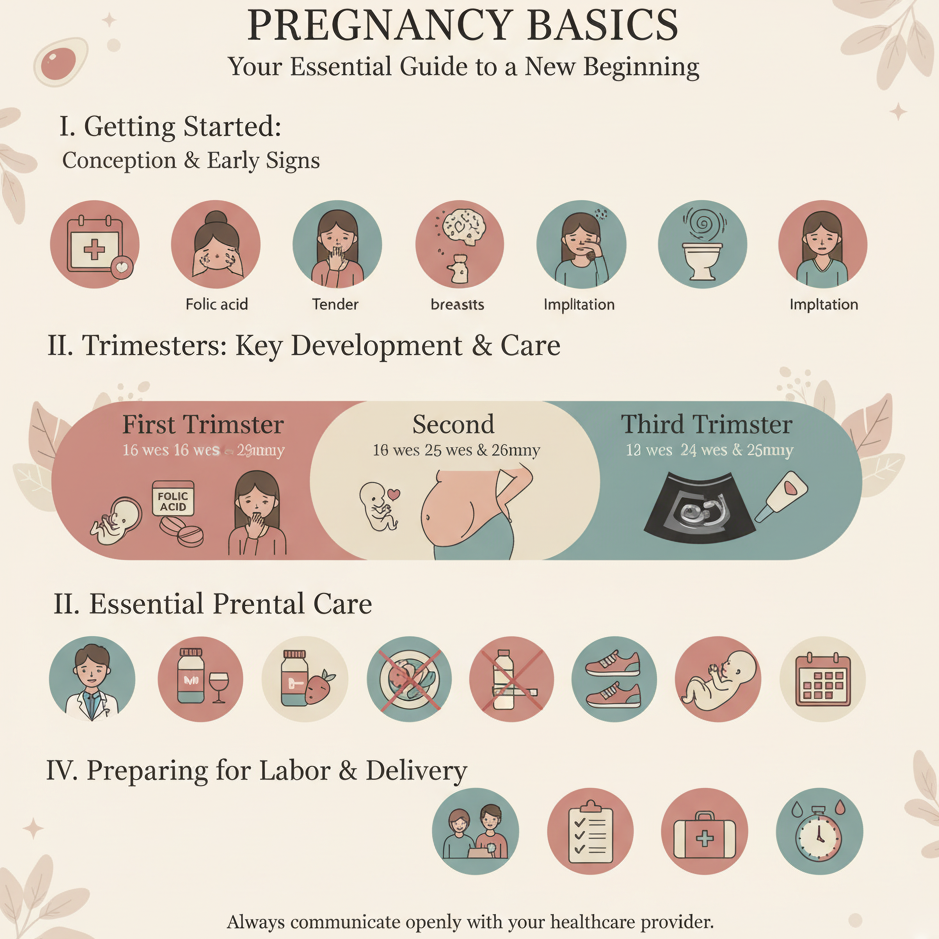
Pregnancy Basics

Week 33 - Fat Accumulation

Week 9 - Fetal Movement Starts

Pregnancy Goal Setting

Week 15 - Hair Growth Begins

Week 19 - Muscle Development
Self-Love Affirmations