Pregnancy Intimacy Guide
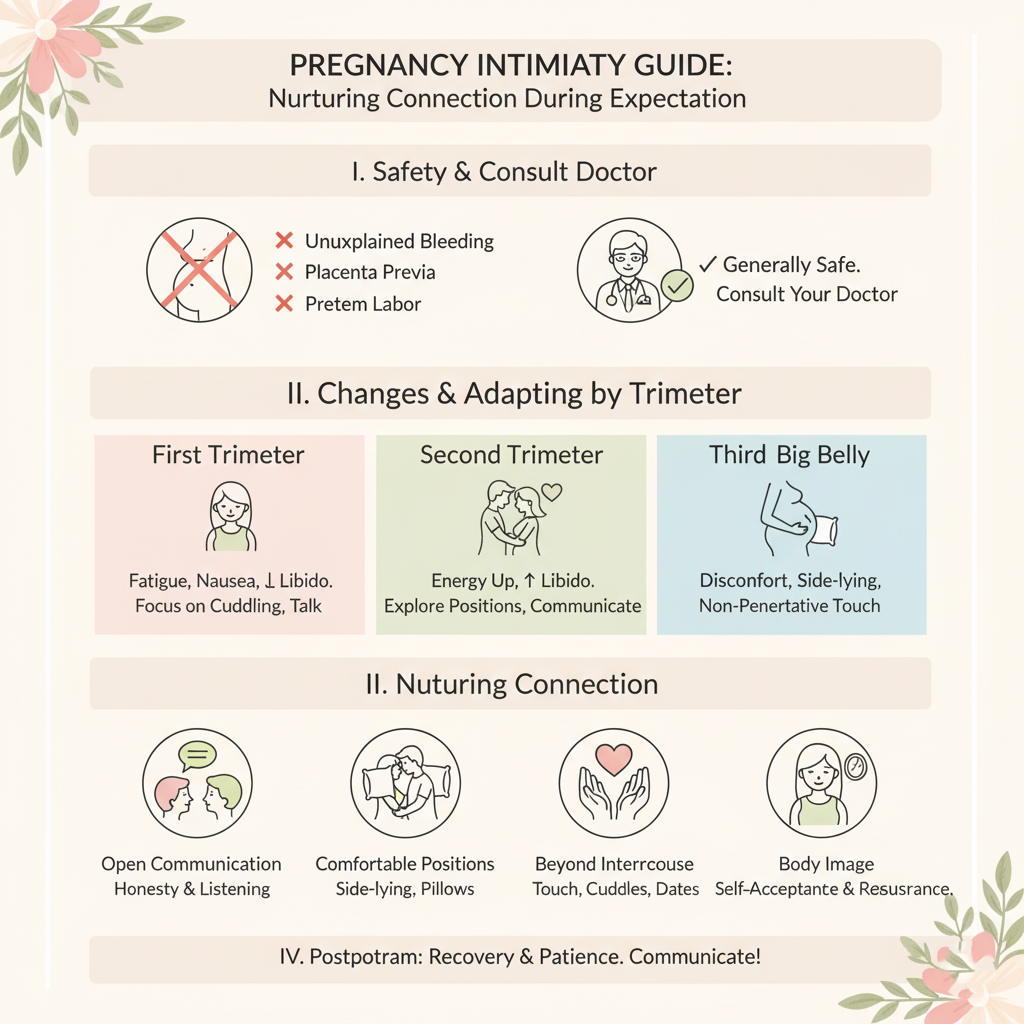
Maintaining intimacy during pregnancy fosters emotional connection, reduces stress, and supports a healthy partnership. Hormonal, physical, and emotional changes can affect intimacy, so this guide provides practical strategies to navigate these shifts safely and comfortably. Always consult a healthcare provider to ensure intimacy is safe for your pregnancy, especially if you have high-risk conditions like preterm labor risk or placenta previa.
1. Understand Intimacy Changes During Pregnancy
-
First Trimester (Weeks 1–12):
-
Changes: Fatigue, nausea, or breast tenderness may reduce desire. Hormonal shifts (e.g., rising estrogen, progesterone) can heighten sensitivity or libido in some.
-
Emotional Impact: Anxiety about pregnancy or body changes may affect closeness.
-
-
Second Trimester (Weeks 13–26):
-
Changes: Increased energy and blood flow to the pelvic area may boost libido. Physical comfort often improves, enhancing intimacy.
-
Emotional Impact: Growing connection to the baby can strengthen partner bonding.
-
-
Third Trimester (Weeks 27–40):
-
Changes: Physical discomfort (e.g., belly size, back pain) or fatigue may reduce desire. Hormonal shifts may vary libido.
-
Emotional Impact: Anticipation of labor may cause stress or deepen emotional intimacy.
-
-
Purpose: Recognizing trimester-specific changes helps tailor intimacy approaches to your needs.
2. Foster Emotional Intimacy
-
Actions:
-
Schedule regular check-ins with your partner to discuss feelings, pregnancy milestones, or concerns (e.g., 10-minute daily talks).
-
Practice affirmations together (e.g., “We are growing stronger as a team”) to reinforce connection.
-
Share activities like reading about pregnancy or attending prenatal visits together.
-
-
Tips:
-
Use journaling to process emotions and share entries with your partner.
-
Express appreciation for each other to build trust and closeness.
-
-
Purpose: Strengthens partnership and supports emotional well-being during pregnancy.
3. Navigate Physical Intimacy Safely
-
Safety Guidelines:
-
Intimacy is generally safe during a healthy pregnancy unless advised otherwise by your healthcare provider.
-
Avoid positions that put pressure on the abdomen (e.g., missionary in later trimesters).
-
Stop if you experience pain, bleeding, or contractions, and contact your provider.
-
-
Comfortable Positions:
-
Side-Lying: Lie on your side with your partner behind (spooning) to minimize belly pressure.
-
Seated or Edge of Bed: Sit on the edge of a bed or chair for comfort and control.
-
Partner on Top: Use pillows to support your back or hips in early trimesters.
-
-
Tips:
-
Use pillows (e.g., pregnancy pillow) for support and comfort.
-
Communicate openly about comfort levels and preferences.
-
-
Purpose: Ensures physical intimacy is safe, comfortable, and enjoyable.
4. Address Common Intimacy Concerns
-
Low Libido:
-
Caused by fatigue, nausea, or body image concerns. Focus on non-physical intimacy (e.g., cuddling, massage) to maintain closeness.
-
-
Body Image:
-
Hormonal or physical changes (e.g., weight gain, stretch marks) may affect confidence. Use affirmations (e.g., “My body is strong and beautiful”) to boost self-esteem.
-
-
Discomfort:
-
Manage back pain or pelvic pressure with heat therapy (10–20 minutes, low heat) or gentle stretching before intimacy.
-
-
Tips:
-
Communicate openly with your partner about fears or discomfort.
-
Explore alternative forms of intimacy (e.g., holding hands, shared relaxation) if physical intimacy feels challenging.
-
-
Purpose: Reduces anxiety and fosters connection despite physical or emotional barriers.
5. Track Intimacy and Emotional Connection
-
Action: Use a notebook, calendar, or digital reminder system to log:
-
Intimacy moments (e.g., “Week 20: shared a relaxing evening, felt connected”).
-
Emotional or physical barriers (e.g., fatigue, discomfort) and coping strategies.
-
Related symptoms (e.g., mood swings, stress) to identify patterns.
-
-
Tips:
-
Note what strengthens connection (e.g., “Talking about baby names boosted mood”).
-
Track for 3–6 months to assess intimacy trends across trimesters.
-
-
Purpose: Helps identify effective strategies and areas needing adjustment for a stronger partnership.
6. Practice Relaxation Together
-
Techniques:
-
Try partner-assisted deep breathing (5 minutes, inhaling/exhaling together) to reduce stress and enhance closeness.
-
Engage in light massage (e.g., back or feet) using unscented lotion to ease pregnancy discomfort.
-
Practice guided meditation together (5–10 minutes) to promote relaxation.
-
-
Tips:
-
Create a calming environment with dim lighting or soft music.
-
Alternate roles (e.g., one partner leads breathing one day, the other the next).
-
-
Purpose: Combines stress relief with intimacy, fostering emotional and physical connection.
7. Communicate Openly with Your Partner
-
Actions:
-
Discuss desires, concerns, or boundaries openly (e.g., “I feel tired but want to stay connected”).
-
Share pregnancy milestones (e.g., fetal movements) to deepen emotional intimacy.
-
Address fears about intimacy (e.g., safety, body image) to build trust.
-
-
Tips:
-
Set aside time weekly for uninterrupted conversations.
-
Use “I” statements (e.g., “I feel anxious about my body”) to express needs clearly.
-
-
Purpose: Strengthens mutual understanding and maintains a supportive partnership.
8. Know When to Seek Medical Advice
-
Warning Signs:
-
Pain, bleeding, or contractions during or after intimacy.
-
Persistent discomfort or emotional distress affecting intimacy.
-
Concerns about safety in high-risk pregnancies (e.g., placenta previa, preterm labor risk).
-
-
Action: Consult a healthcare provider immediately if you experience concerning symptoms or have questions about intimacy safety.
-
High-Risk Pregnancies: Discuss intimacy guidelines with your provider if you have conditions like hypertension or a history of miscarriage.
-
Purpose: Ensures intimacy is safe and addresses underlying health concerns.
Benefits
-
Stronger Partnership: Enhances emotional and physical closeness during pregnancy.
-
Stress Reduction: Lowers cortisol, supporting maternal and fetal health.
-
Emotional Well-Being: Boosts confidence and reduces pregnancy-related anxiety.
Practical Tips
-
Tracking Tools: Log intimacy moments and emotional outcomes in a journal (e.g., “Week 15: tried side-lying position, felt comfortable”). Include symptoms for provider discussions.
-
Environment Setup: Create a relaxing space with pillows, dim lighting, or calming scents (e.g., lavender, if safe) for intimacy or relaxation.
-
Communication Starters: Use prompts like “What makes you feel close to me?” to spark intimacy discussions.
-
Comfort Aids: Keep pillows or a warm water bottle handy for physical comfort during intimacy or relaxation.
-
Nutrition Support: Eat balanced meals with mood-stabilizing nutrients (e.g., omega-3s from walnuts) to support emotional health.
-
Partner Involvement: Plan intimacy-focused activities (e.g., a shared bath, massage) weekly to maintain connection.
Actionable Next Steps
-
Today: Choose a tracking tool and discuss one intimacy goal with your partner (e.g., more emotional check-ins).
-
This Week: Try a relaxation technique together (e.g., 5-minute breathing) and log its impact.
-
Ongoing: Track intimacy practices and emotional connection across trimesters. Consult your provider for any concerns about safety or comfort.
Related Articles

Implantation calculator

Week 36 - Descent into Pelvis

Ovulation Calculator

Week 19 - Muscle Development
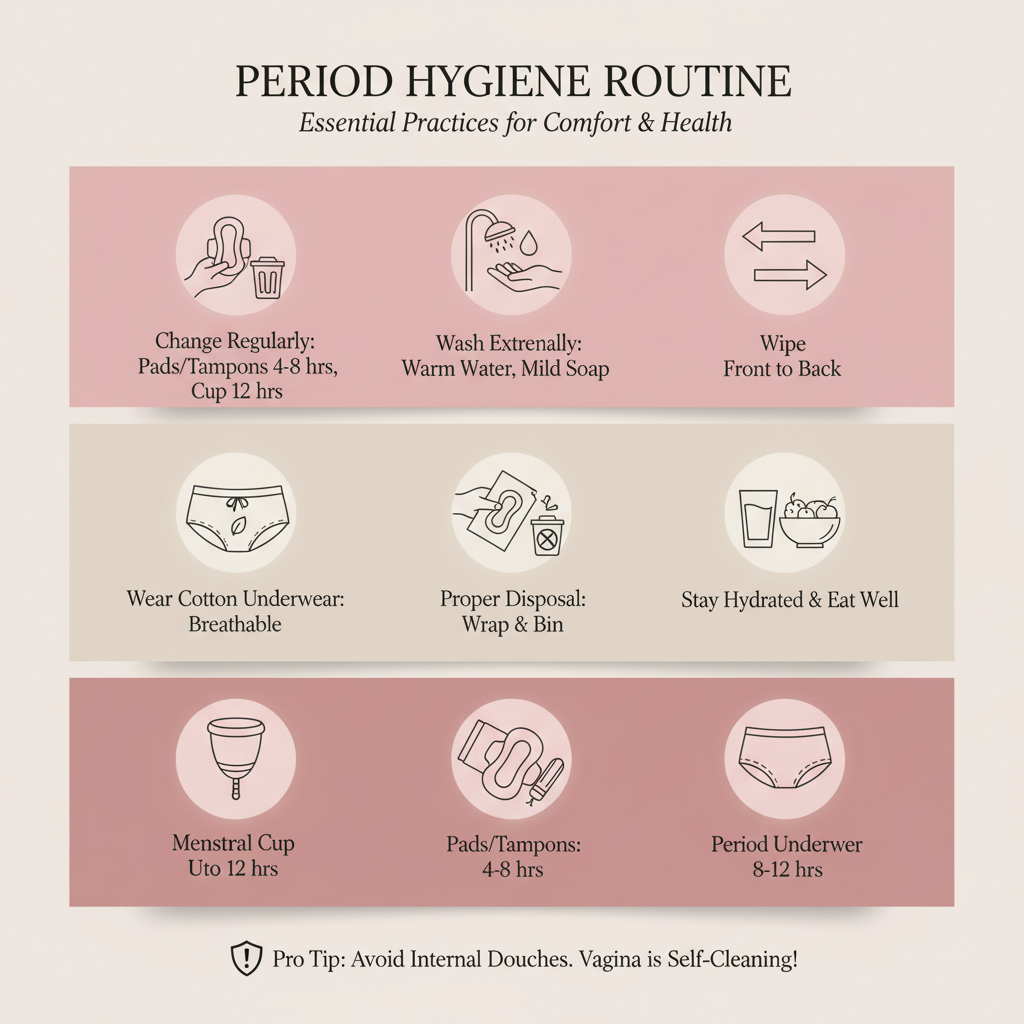
Period Hygiene Routine

Week 29 - Lung Function Improves

Week 21 - Eyebrows Form

Week 16 - Mid-Pregnancy Milestone