Fertility Test Basics: Your Guide to Tracking Pregnancy
Fertility tests offer valuable insights when conception takes longer than expected. This guide outlines the process, timing, and benefits of fertility testing to support your family-building journey.
1. When to Start Testing
-
General Timeline: Consider fertility testing after 6-12 months of trying to conceive without success.
-
Age Consideration: If you’re over 35, start testing after 6 months due to age-related declines in fertility.
-
Other Triggers: Seek testing sooner if you have irregular cycles, known reproductive issues, or recurrent pregnancy loss.
2. Types of Fertility Tests
For Individuals with Ovaries
-
Hormone Blood Test (Days 2-4 of cycle): Measures levels of hormones like FSH, LH, and AMH to assess ovarian reserve and ovulation potential.
-
Imaging Test (Days 6-11 of cycle): Ultrasound or similar scans check reproductive structures (e.g., ovaries, uterus) for abnormalities like fibroids or cysts.
-
Pelvic Exam: A physical check to identify structural issues or signs of conditions like endometriosis.
For Individuals with Testes
-
Semen Analysis: Evaluates sperm count, motility (movement), and morphology (shape) to assess fertility potential.
-
Physical Exam: Checks for physical issues like varicoceles that may affect sperm production.
3. First Steps Before Testing
-
Lifestyle Review: Assess factors like diet, exercise, smoking, alcohol, or stress, as these can impact fertility.
-
Medical History: Share details of past surgeries, medications, or health conditions with your healthcare provider.
-
Track Symptoms: Log cycle details, ovulation signs, or other symptoms in a notebook or app to provide context for tests.
Tip: Use a simple fertility journal to record lifestyle habits and test results for easy reference during consultations.
4. Benefits of Fertility Testing
-
Early Detection: Identifies issues like low ovarian reserve, hormonal imbalances, or low sperm count early, enabling timely interventions.
-
Personalized Plans: Test results guide tailored treatment options, such as medication, lifestyle changes, or assisted reproductive techniques.
-
Reduced Uncertainty: Clear data helps you understand your fertility status and make informed decisions.
5. Pro Tips for Success
-
Work with a Specialist: Consult a healthcare provider with expertise in fertility to ensure accurate testing and interpretation.
-
Track Results: Keep a detailed log of test outcomes, dates, and follow-up plans to stay organized.
-
Stay Consistent: Complete all recommended tests, even if initial results are normal, to get a full picture.
-
Support System: Discuss results with your partner or a trusted person to reduce stress and plan next steps together.
6. When to Seek Further Help
Contact a healthcare provider if tests reveal:
-
Abnormal hormone levels, low sperm count, or structural issues.
-
Persistent challenges conceiving after initial treatments.
-
Emotional or physical strain affecting your well-being.
7. Why It’s Worth It
Fertility testing provides clarity and direction, reducing guesswork in your journey to parenthood. By understanding your body’s unique needs, you can take proactive steps toward building your family with confidence.
Start Today: Schedule a consultation with a healthcare provider to discuss your fertility goals and begin testing when ready!
Related Articles

Week 5 - Heartbeat Begins
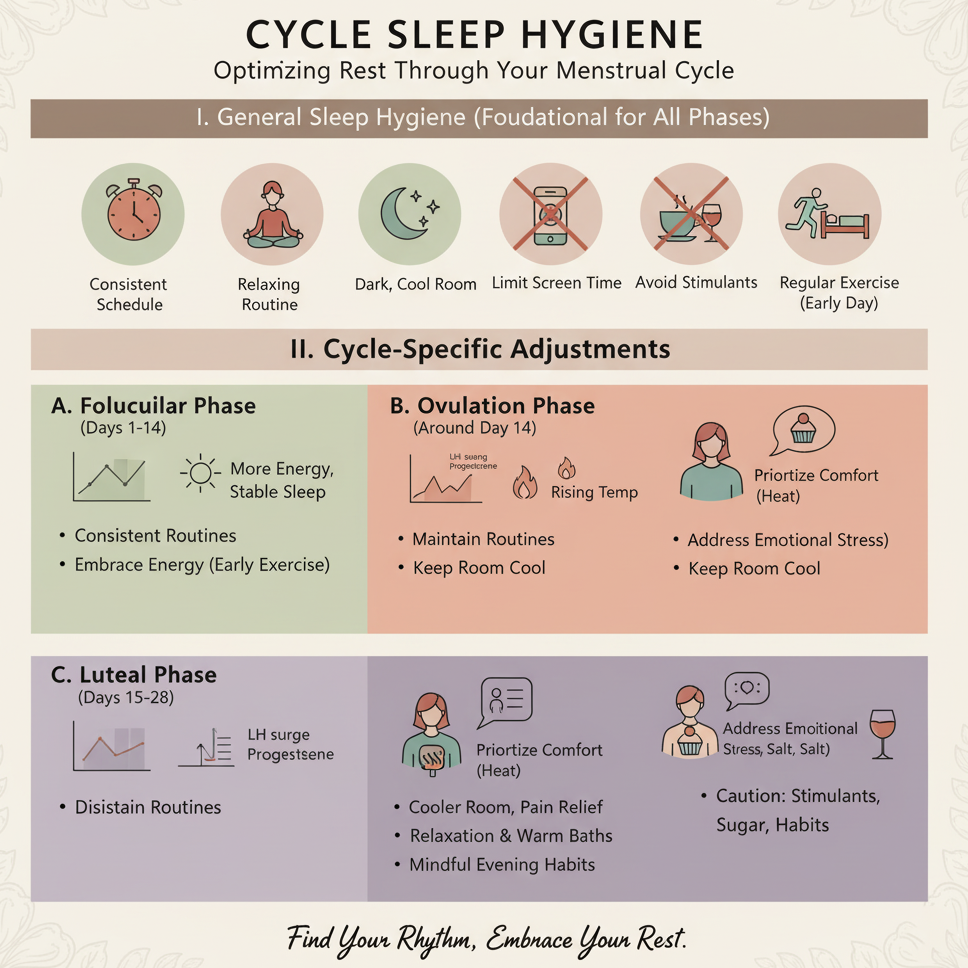
Cycle Sleep Hygiene

Week 39 - Final Growth

Pregnancy Test Calculator
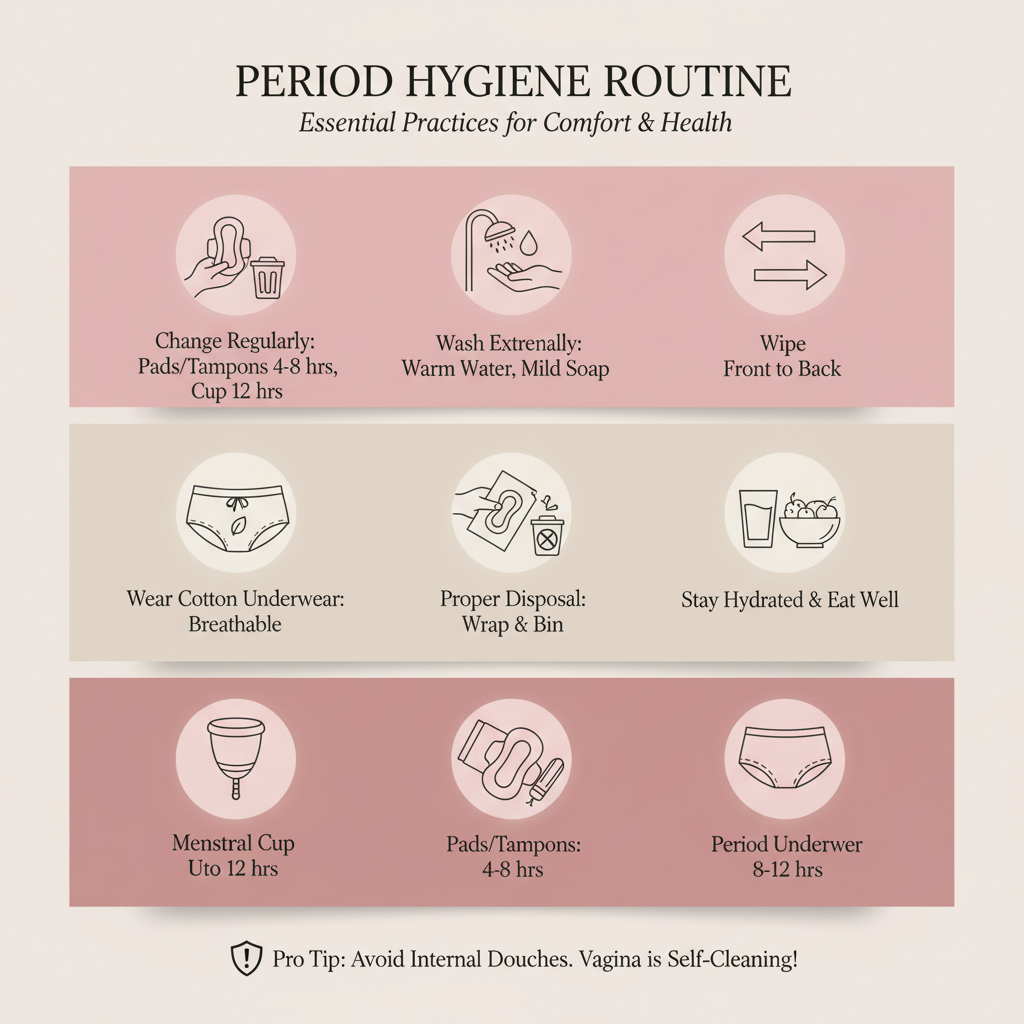
Period Hygiene Routine

Pregnancy Nap Tips
Stress Relief Techniques

Week 34 - Immune System Develops