Fertility Signs

Recognizing fertility signs through consistent cycle tracking empowers you to plan or prevent pregnancy effectively. By monitoring key indicators, you can identify your fertile window and gain insights into reproductive health. Always consult a healthcare provider if you notice irregularities or have concerns about fertility.
1. Choose a Tracking Tool
Select a simple tool, such as a notebook, calendar, or digital reminder system, to record your cycle start dates and fertility signs. Consistent logging over multiple cycles helps establish a personalized pattern for predicting fertile days.
2. Key Fertility Signs
Track these physical indicators daily to pinpoint your fertile window:
-
Cervical Mucus: Observe changes in mucus consistency. During fertile days (typically days 10-14 in a 28-day cycle), mucus becomes clear, stretchy, and egg-white-like, indicating peak fertility.
-
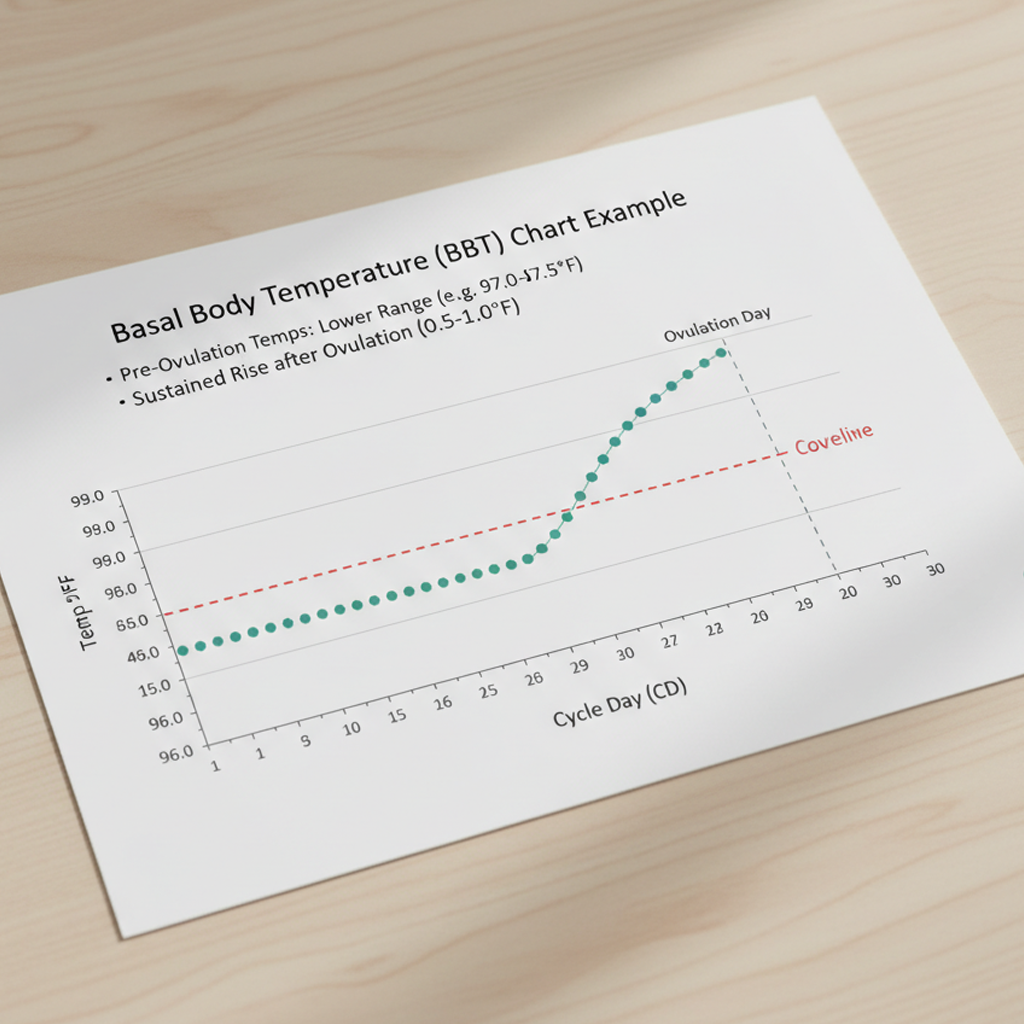
Basal Body Temperature (BBT): Measure your temperature each morning before getting out of bed using a sensitive thermometer (accurate to 0.1°F or 0.1°C). A rise of 0.5-1°F (0.3-0.6°C) typically occurs after ovulation, signaling the end of the fertile window.
-
Mid-Cycle Pain: Note mild pelvic or abdominal discomfort (known as mittelschmerz), which some experience during ovulation.
-
Additional Signs: Record libido spikes or breast tenderness, which may align with fertile days.
3. Track Consistently
-
Log data for 3-6 months to build a reliable pattern, as stress, illness, or lifestyle changes can affect cycle timing.
-
Consistency improves accuracy, especially for irregular cycles.
4. Enhance Accuracy with Predictor Kits
-
Use over-the-counter ovulation predictor kits to detect a luteinizing hormone (LH) surge, which occurs 12-36 hours before ovulation. Follow the kit’s instructions for accurate testing.
-
Combine kits with symptom tracking to confirm fertile days, especially when trying to conceive.
5. Monitor for Irregularities
-
If fertility signs are inconsistent, absent, or cycles vary by more than 7 days, consult a healthcare provider. This may indicate conditions like low ovarian reserve or hormonal imbalances.
-
Seek medical advice for persistent irregular cycles, severe pain, or difficulty conceiving after 6-12 months of trying (or sooner if over 35).
Benefits
-
Natural Family Planning: Identifying fertile days supports conception or natural contraception methods.
-
Early Issue Detection: Tracking reveals potential fertility concerns, enabling timely medical evaluation.
-
Body Literacy: Understanding your cycle fosters informed reproductive choices.
Practical Tips
-
Tracking Tools: Use a paper calendar, spreadsheet, or phone-based reminder to log cycle days and symptoms. Choose a method that’s easy to maintain daily.
-
BBT Measurement: Use a digital thermometer designed for BBT. Measure at the same time each morning before any activity for consistent data.
-
Cervical Mucus Observation: Check mucus daily, ideally at a consistent time (e.g., after a shower). Note changes in color, texture, and quantity.
-
Predictor Kits: Test urine during the estimated fertile window (e.g., days 10-17 for a 28-day cycle) to detect the LH surge. Store kits in a cool, dry place for accuracy.
-
Lifestyle Factors: Stress, poor sleep, or dietary changes can disrupt cycles. Maintain a balanced diet and moderate exercise to support reproductive health.
-
Irregular Cycles: For unpredictable cycles, track symptoms diligently and consult a healthcare provider for tests like hormone panels or ultrasounds.
Actionable Next Steps
-
Today: Select a tracking tool and begin logging the first day of your current or next period.
-
This Week: Start monitoring daily fertility signs (mucus, BBT, pain, libido, or tenderness).
-
Over the Next 3-6 Months: Track consistently to establish patterns. Consider using a predictor kit during your fertile window.
-
Ongoing: Review data regularly and consult a healthcare provider if signs are inconsistent or you have conception concerns.
Related Articles

Week 24 - Viability Threshold

Week 27 - End of Second Trimester

Ovulation Calculator

Week 12 - End of First Trimester
Fertility Test Basics: Your Guide to Tracking Pregnancy

Exercise for Period Pain

Pregnancy Goal Setting
Week 18 - Hearing Develops