Cycle Phase Overview
Understanding the phases of the menstrual cycle is essential for tracking fertility, planning pregnancy, or monitoring reproductive health. Each phase involves distinct hormonal and physical changes that influence ovulation and conception. By logging cycle details, you can identify fertile windows and detect potential irregularities. Always consult a healthcare provider if you notice abnormal patterns or have concerns about your cycle.
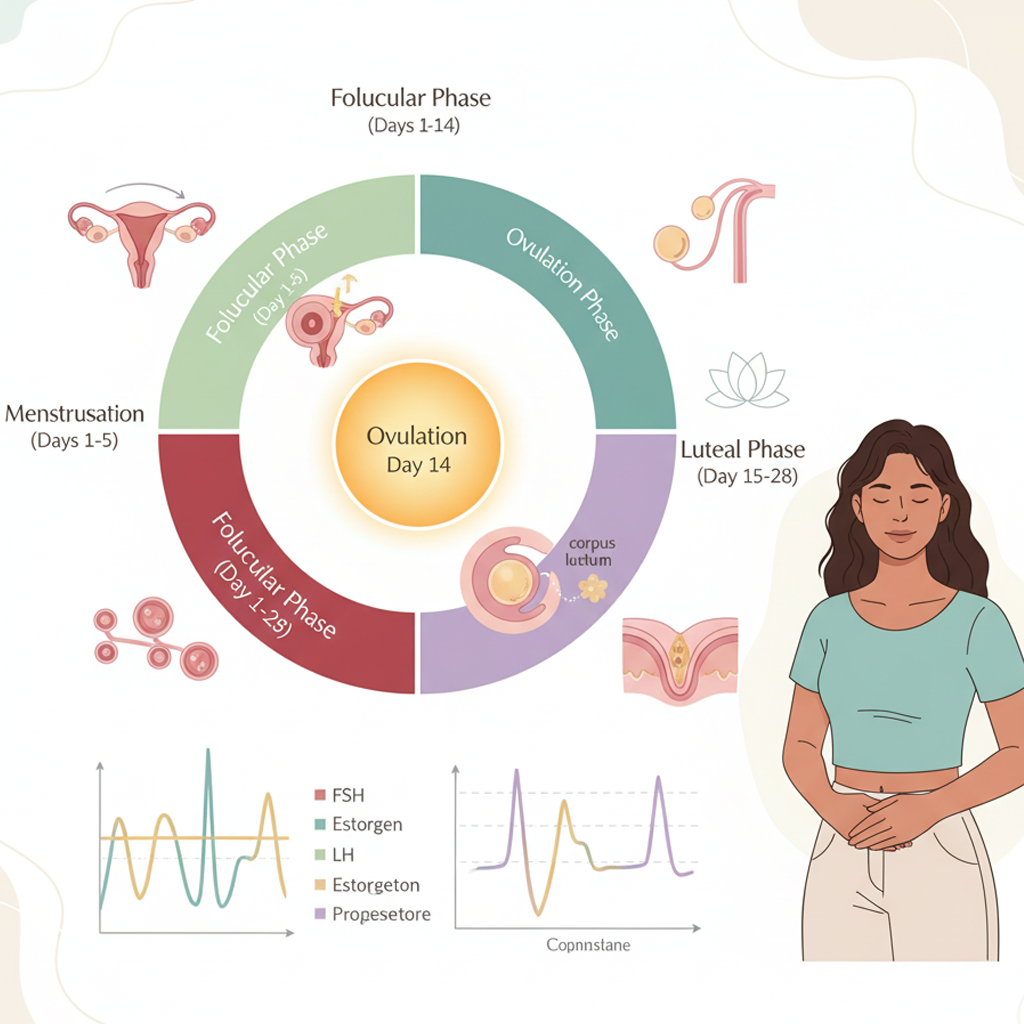
1. Overview of the Menstrual Cycle
-
Definition: The menstrual cycle is the monthly process preparing the body for potential pregnancy, typically lasting 21–35 days (28 days on average).
-
Phases: The cycle consists of four main phases: Menstrual, Follicular, Ovulation, and Luteal.
-
Purpose: Tracking these phases helps optimize conception timing, supports natural contraception, or identifies hormonal imbalances.
2. Menstrual Phase (Days 1–5, varies)
-
Description: Begins on the first day of menstruation (day 1), when the uterine lining sheds if no pregnancy occurs.
-
Hormonal Changes:
-
Estrogen and progesterone levels are low, triggering the shedding of the endometrium.
-
Follicle-stimulating hormone (FSH) starts to rise, preparing for follicle development.
-
-
Physical Signs:
-
Vaginal bleeding (light to heavy flow, lasting 3–7 days).
-
Possible cramping, fatigue, or mood changes.
-
-
Tracking Tips:
-
Log the start date, flow intensity (e.g., light, moderate, heavy), and symptoms like cramps in a notebook or digital reminder system.
-
Note cycle length variations to establish your baseline.
-
-
Purpose: Marks the cycle’s start and signals the body to begin preparing for ovulation.
3. Follicular Phase (Days 1–13, varies)
-
Description: Begins on day 1 (overlaps with menstruation) and continues until ovulation. The body prepares follicles (egg-containing sacs) for release.
-
Hormonal Changes:
-
FSH stimulates follicle growth in the ovaries.
-
Estrogen levels rise, thickening the uterine lining for potential implantation.
-
-
Physical Signs:
-
Cervical mucus transitions from dry/sticky (post-menstruation) to creamy or wet as ovulation nears.
-
Energy levels may increase after menstruation ends.
-
-
Tracking Tips:
-
Record cervical mucus changes daily (e.g., sticky, creamy) in a log.
-
Measure basal body temperature (BBT) each morning with a digital thermometer (accurate to 0.1°F or 0.1°C) to establish a baseline (typically lower in this phase).
-
-
Purpose: Prepares the body for ovulation and supports fertility awareness.
4. Ovulation Phase (Day 14, varies)
-
Description: The release of a mature egg from the ovary, typically occurring mid-cycle (around day 14 in a 28-day cycle). This is the most fertile phase.
-
Hormonal Changes:
-
A surge in luteinizing hormone (LH) triggers egg release.
-
Estrogen peaks just before ovulation, enhancing cervical mucus fertility.
-
-
Physical Signs:
-
Cervical mucus becomes clear, stretchy, and egg-white-like, indicating peak fertility (days 10–14 in a 28-day cycle).
-
A slight rise in BBT (0.5–1°F or 0.3–0.6°C) occurs post-ovulation.
-
Mild pelvic or abdominal pain (mittelschmerz) in some cases.
-
Possible libido spikes or breast tenderness.
-
-
Tracking Tips:
-
Use over-the-counter ovulation predictor kits to detect the LH surge (12–36 hours before ovulation). Test urine daily during the estimated fertile window (e.g., days 10–17).
-
Log cervical mucus, BBT, and any pain or mood changes to confirm ovulation timing.
-
-
Purpose: Identifies the fertile window (typically 5 days before ovulation plus the day of ovulation) for conception or natural contraception.
5. Luteal Phase (Days 15–28, varies)
-
Description: Begins after ovulation and lasts until the next period or pregnancy. The body prepares for potential implantation or cycle reset.
-
Hormonal Changes:
-
Progesterone rises, maintaining the uterine lining for implantation.
-
Estrogen remains elevated but lower than at ovulation.
-
If no pregnancy occurs, both hormones drop, triggering menstruation.
-
-
Physical Signs:
-
Cervical mucus becomes sticky or dry.
-
BBT remains elevated (0.5–1°F higher than follicular phase) until just before menstruation.
-
Possible premenstrual symptoms (e.g., bloating, mood swings, breast tenderness).
-
-
Tracking Tips:
-
Continue logging BBT to confirm the luteal phase length (typically 10–16 days).
-
Note premenstrual symptoms to anticipate the next cycle or detect early pregnancy signs (e.g., sustained high BBT).
-
-
Purpose: Supports implantation or prepares the body for the next cycle.
6. Monitor for Irregularities
-
Signs to Watch:
-
Cycles shorter than 21 days or longer than 35 days.
-
Absent or irregular ovulation signs (e.g., no LH surge, inconsistent mucus changes).
-
Severe pain, heavy bleeding, or persistent symptoms like fatigue or mood changes.
-
-
Action: Consult a healthcare provider if cycles vary by more than 7 days, ovulation signs are absent, or conception is unsuccessful after 6–12 months (6 months if over 35). These may indicate conditions like polycystic ovary syndrome (PCOS) or thyroid issues.
-
Purpose: Ensures early detection of reproductive health concerns.
Benefits
-
Fertility Awareness: Identifies fertile windows for conception or natural contraception.
-
Cycle Health Insights: Reveals patterns to detect hormonal imbalances early.
-
Empowered Planning: Enhances understanding of your body for informed reproductive choices.
Practical Tips
-
Tracking Tools: Use a paper calendar, notebook, or phone-based reminder to log cycle start dates, symptoms, and fertility signs. Record daily for 3–6 months to establish patterns.
-
BBT Measurement: Use a digital thermometer to measure BBT each morning before rising. Note results to track temperature shifts across phases.
-
Cervical Mucus Observation: Check mucus daily at a consistent time (e.g., after a shower). Record texture (e.g., sticky, creamy, egg-white-like) and color.
-
Ovulation Kits: Test urine during the estimated fertile window (e.g., days 10–17 for a 28-day cycle) to detect the LH surge. Store kits in a cool, dry place for accuracy.
-
Lifestyle Support: Maintain a balanced diet, moderate exercise (150 minutes weekly), and stress management (e.g., 10-minute meditation) to support cycle regularity.
-
Partner Involvement: Share cycle tracking with your partner to align conception efforts or discuss irregularities for joint decision-making.
Actionable Next Steps
-
Today: Choose a tracking tool and log the first day of your current or next period.
-
This Week: Begin monitoring daily fertility signs (e.g., cervical mucus, BBT) and symptoms like pain or mood changes.
-
Next 3–6 Months: Track consistently to map your cycle phases and fertile windows. Consider using an ovulation predictor kit mid-cycle.
-
Ongoing: Review patterns and consult a healthcare provider if you notice irregularities or have conception concerns.
Related Articles
Week 1 - Early Pregnancy

Week 19 - Muscle Development

Week 14 - Bones Harden

Week 8 - Major Organs Develop
Self-Love Affirmations

Week 36 - Descent into Pelvis

Week 10 - Fingernails Form
Week 31 - Bone Strengthening