Pregnancy Wellness Tips
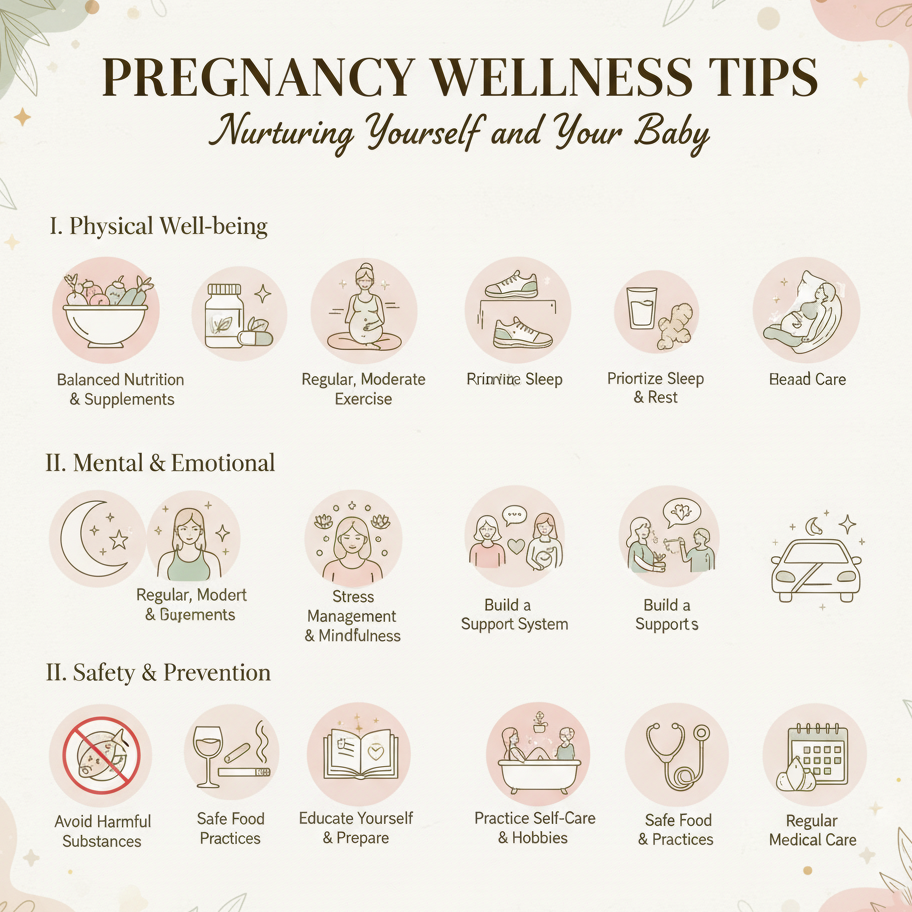
Maintaining wellness during pregnancy supports maternal health, fetal development, and emotional resilience. This guide provides practical strategies to promote physical, mental, and emotional well-being across all trimesters. Always consult a healthcare provider to tailor these tips to your individual needs, especially if you have conditions like gestational diabetes, hypertension, or a history of preterm birth.
1. Prioritize Balanced Nutrition
-
Action: Eat a nutrient-rich diet with:
-
Folic Acid (400–800 mcg daily): Leafy greens (spinach), legumes, and prenatal vitamins to prevent neural tube defects.
-
Iron (27 mg daily): Lean meats, spinach, and lentils to support blood volume and prevent anemia.
-
Calcium (1,000 mg daily): Dairy, fortified plant-based milk, or broccoli for fetal bone development.
-
Protein (70–100 g daily): Eggs, tofu, or chicken for tissue growth.
-
Omega-3s (200–300 mg DHA daily): Salmon, walnuts, or chia seeds for brain development.
-
-
Tips:
-
Aim for 2.5–3 cups of vegetables, 1.5–2 cups of fruits, and 6–8 oz of whole grains daily.
-
Limit caffeine to under 200 mg (one 8 oz coffee) and avoid alcohol completely.
-
-
Purpose: Supports fetal growth and maternal energy, reducing risks like anemia or developmental issues.
2. Stay Active with Safe Exercise
-
Action: Engage in 150 minutes of moderate exercise weekly (e.g., walking, swimming, prenatal yoga), unless contraindicated by your provider.
-
Benefits: Improves circulation, reduces swelling, and boosts mood via endorphins.
-
Tips:
-
Avoid high-impact activities or exercises with a fall risk (e.g., contact sports) in later trimesters.
-
Stop if you experience pain, dizziness, or shortness of breath, and consult your provider.
-
-
Purpose: Enhances physical health and prepares the body for labor and delivery.
3. Manage Stress and Emotional Health
-
Techniques:
-
Practice 5–10 minutes of deep breathing or mindfulness meditation daily to lower cortisol.
-
Use self-love affirmations (e.g., “I am nurturing my baby with strength”) to boost confidence.
-
Journal thoughts or emotions to process pregnancy-related changes or anxieties.
-
-
Tips:
-
Set aside a daily relaxation period (e.g., evening wind-down) in a calm environment.
-
Connect with a support group of expectant parents for shared experiences.
-
-
Purpose: Reduces stress-related risks like irregular cycles pre-pregnancy or complications during pregnancy.
4. Prioritize Sleep and Rest
-
Action: Aim for 7–9 hours of sleep nightly, plus 20–60-minute naps if needed, especially in the first and third trimesters.
-
Tips:
-
Sleep on your left side with a pregnancy pillow to support your belly and improve blood flow.
-
Create a restful environment (cool, dark, quiet) and limit screen time before bed.
-
-
Purpose: Combats fatigue, supports hormonal balance, and enhances fetal development.
5. Track Symptoms and Wellness Practices
-
Action: Use a notebook, calendar, or digital reminder system to log:
-
Nutrition (e.g., daily intake of key nutrients like iron or calcium).
-
Exercise (e.g., “30-min walk, felt energized”).
-
Stress levels and relief techniques (e.g., meditation outcomes).
-
Symptoms like nausea, fatigue, or fetal movements (second trimester onward).
-
-
Tips:
-
Note patterns (e.g., “nausea worse after fatty meals”) to discuss with your provider.
-
Track fetal movements daily (aim for 10 in 2 hours by week 28) to monitor baby’s health.
-
-
Purpose: Helps identify trends, optimize wellness, and communicate effectively with your healthcare provider.
6. Stay Hydrated
-
Action: Drink 8–10 cups (2–2.5 liters) of water daily to support digestion, reduce swelling, and maintain amniotic fluid levels.
-
Tips:
-
Carry a reusable water bottle for consistent hydration.
-
Add lemon or cucumber slices for flavor if plain water feels unappealing.
-
-
Purpose: Prevents dehydration, which can worsen fatigue or trigger contractions.
7. Attend Regular Prenatal Checkups
-
Action: Schedule and attend prenatal visits as recommended (e.g., monthly until week 28, biweekly until week 36, then weekly).
-
Tips:
-
Bring your symptom and wellness log to discuss nutrition, exercise, or emotional health.
-
Ask about tests (e.g., ultrasounds, glucose screening) to monitor fetal growth and maternal health.
-
-
Purpose: Ensures early detection of issues and supports tailored wellness plans.
8. Involve Your Partner or Support System
-
Action:
-
Share wellness goals (e.g., meal planning, exercise routines) with your partner for mutual accountability.
-
Discuss emotional needs or stressors to build a supportive environment.
-
-
Tips:
-
Plan healthy meals together or join a prenatal exercise class as a team.
-
Encourage your partner to adopt similar healthy habits (e.g., balanced diet, stress management).
-
-
Purpose: Strengthens partnership and fosters a supportive pregnancy journey.
9. Know When to Seek Medical Advice
-
Warning Signs:
-
Severe or persistent symptoms (e.g., vomiting, intense pain, reduced fetal movement).
-
Signs of complications like preeclampsia (sudden swelling, severe headache) or preterm labor (regular contractions before 37 weeks).
-
Persistent emotional distress (e.g., anxiety, sadness) not alleviated by wellness practices.
-
-
Action: Contact your healthcare provider immediately for concerning symptoms or if wellness practices aren’t effective.
-
High-Risk Pregnancies: If you have conditions like hypertension or a history of miscarriage, discuss a tailored wellness plan with your provider.
-
Purpose: Ensures timely intervention for maternal or fetal health concerns.
Benefits
-
Optimal Fetal Development: Supports healthy growth of the baby’s brain, bones, and organs.
-
Maternal Well-Being: Reduces fatigue, stress, and pregnancy complications.
-
Confident Preparation: Builds resilience and readiness for labor and parenthood.
Practical Tips
-
Nutrition Planning: Prep nutrient-rich snacks (e.g., yogurt with berries, nuts) for convenience and to manage nausea.
-
Exercise Safety: Wear supportive shoes and stay hydrated during walks or prenatal yoga. Check with your provider for pregnancy-safe activities.
-
Tracking Tools: Log wellness practices in a journal (e.g., “Day 20: ate spinach salad, 30-min walk, felt refreshed”). Include symptoms for provider discussions.
-
Relaxation Space: Create a calming area with pillows, dim lighting, or soft music for meditation or naps.
-
Hydration Habit: Set phone reminders to drink water every 2–3 hours to meet daily goals.
-
Support System: Schedule weekly check-ins with your partner or a friend to discuss wellness progress and emotional needs.
Actionable Next Steps
-
Today: Choose a tracking tool and log your current diet, exercise, or stress levels. Start a prenatal vitamin with folic acid.
-
This Week: Plan a balanced meal with key nutrients and try a 10-minute relaxation technique (e.g., deep breathing).
-
Ongoing: Track wellness practices and symptoms across trimesters. Consult your healthcare provider for any concerning symptoms or to adjust your plan.
Related Articles

Implantation calculator

Cycle Self-Care Rituals

Pregnancy Nap Tips

Week 4 - Neural Tube Development
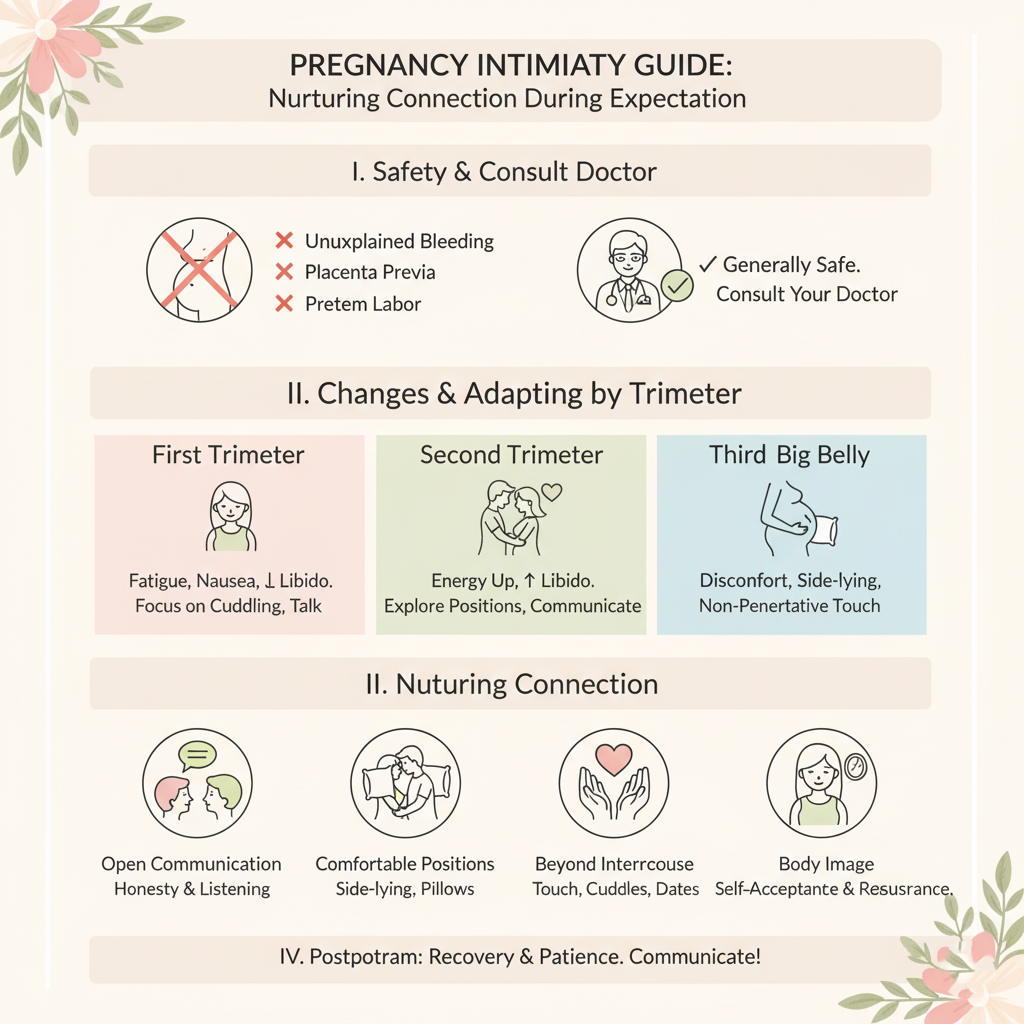
Pregnancy Intimacy Guide

Fertility Signs

Week 33 - Fat Accumulation
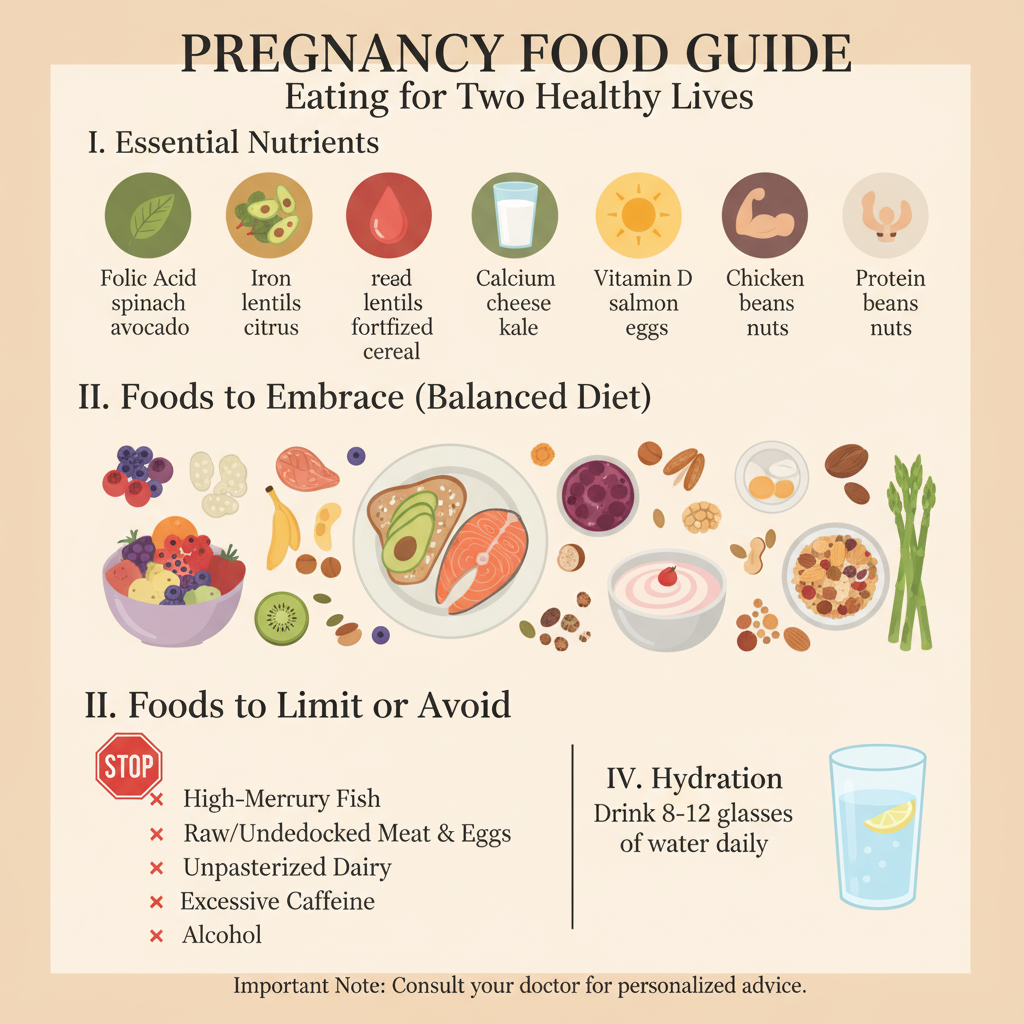
Pregnancy Food Guide